

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2019.v05i03.001
Year: 2019, Volume: 5, Issue: 3, Pages: 1-6
Original Article
K Suman1, Namrata Rao2
1,2Assistant Professor, Department of Pathology, Melaka Manipal Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India
Address for correspondence:
Dr. Namrata Rao, Assistant Professor, Department of Pathology, Melaka Manipal Medical College, Manipal Academy of Higher Education, 14/6, B Type Flats, KMC Campus,
Manipal - 576 104, Karnataka, India. Phone: +91-9844034100. E-mail: [email protected]
Objective: Dyspepsia is a common condition which is seen in the medical outpatient department. Helicobacter pylori is the causal agent in most of the cases of gastritis and peptic ulceration. This is a retrospective study aimed to study the histological patterns in gastric biopsy from patients with complaints of dyspepsia.
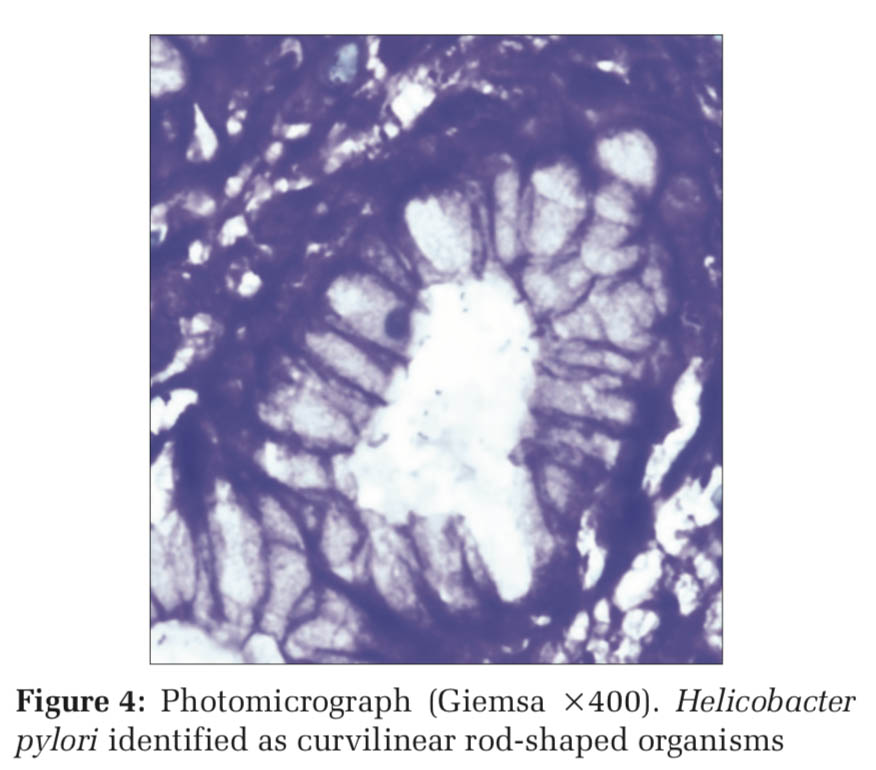
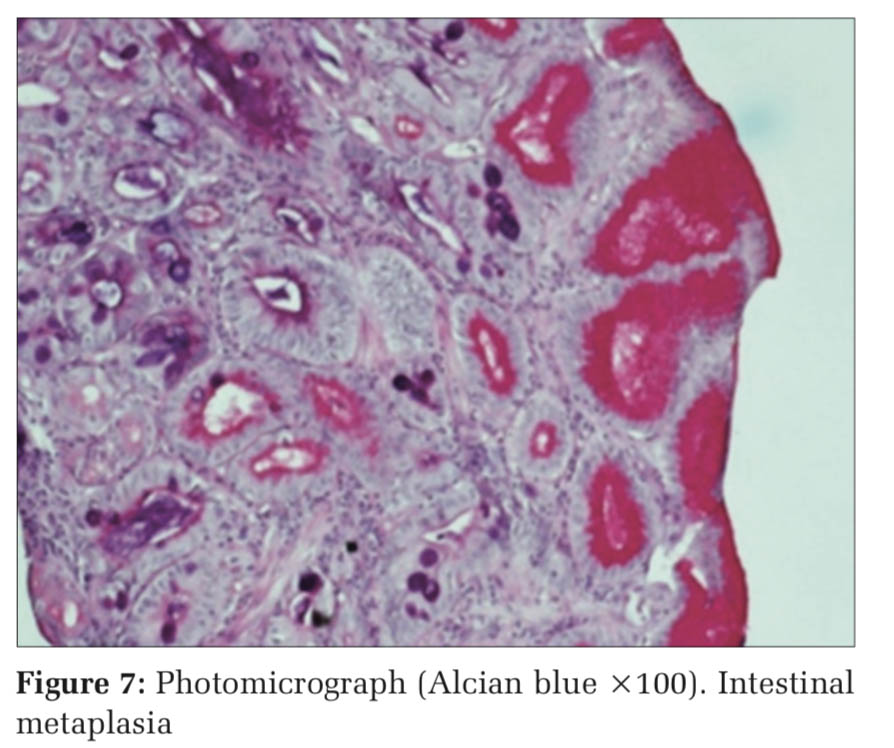
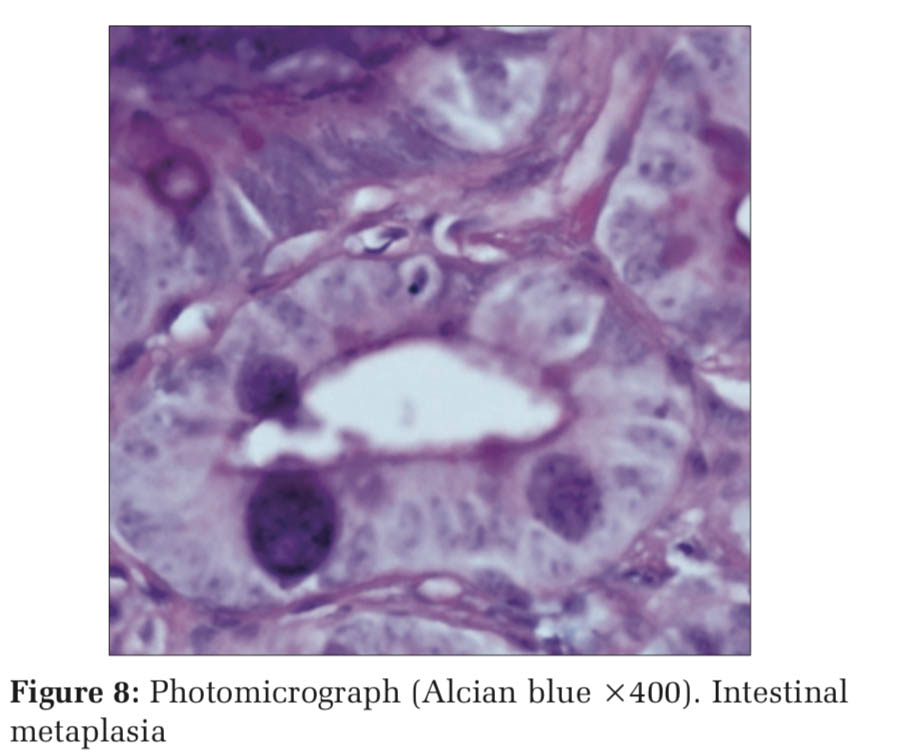
Methods: In this study, a total of 550 biopsy samples from patients with a clinical history of dyspepsia which were received at the department of histopathology were analyzed. The biopsy samples were procured in Bouin’s fixative and were paraffin embedded. Sections were taken and stained with hematoxylin and eosin. May-Grunwald-Giemsa stain was used to visualize H. pylori. Alcian blue stain was used to identify intestinal metaplasia.
Results: It was observed that 194 (35.2%) cases showed features of chronic gastritis without H. pylori infection. H. pylori was noted in a total of 296 cases (53.8%) among which 256 cases (46.5%) showed features of chronic gastritis, 28 cases (5.09%) showed active gastritis, and 12 cases (2.2%) showed features of chronic gastritis with intestinal metaplasia.
Conclusions: Chronic gastritis is a common condition worldwide. Chronic infection with H. pylori accounts for the majority of cases of chronic gastritis.
KEY WORDS:Activity, dyspepsia, gastritis, Helicobacter pylori, inflammation, metaplasia.
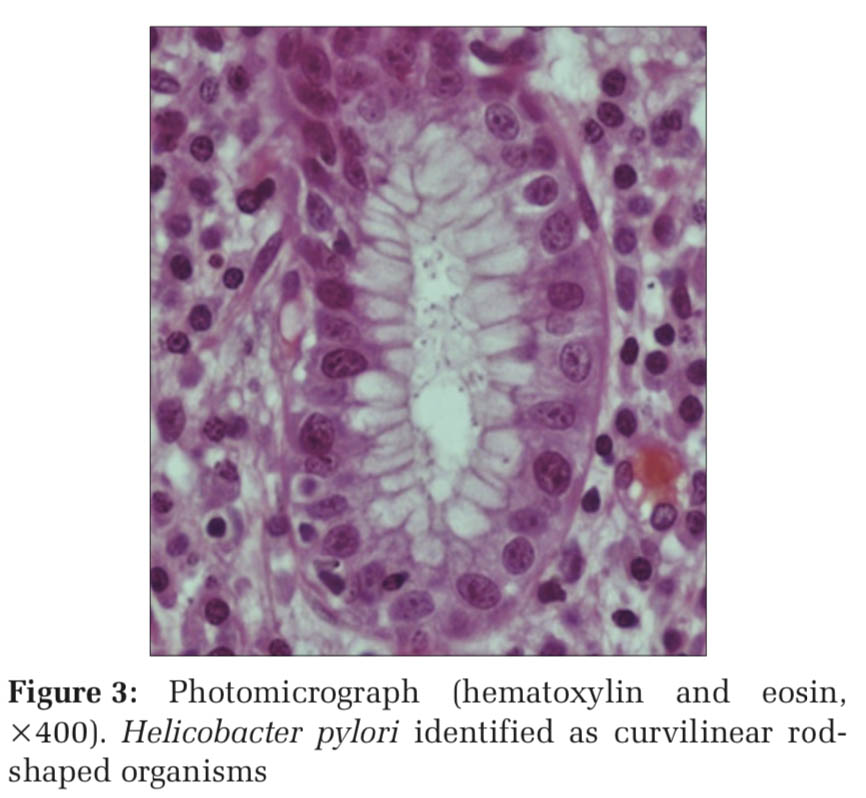
Dyspepsia is one of the most common symptoms presented by patients in general medical and gastroenterology outpatient departments. It is described as recurrent epigastric discomfort and fullness usually after meals. Endoscopy is a valuable investigation for visualization of gastric mucosa and mucosal sampling for histological examination.[1] The modern era of gastrointestinal endoscopy began in 1957 when Basil developed first fiber-optic gastroscope.[2] Helicobacter pylori is the principal- agent linked to the pathogenesis of chronic gastritis and peptic ulceration. Helicobacter is a Gram-negative curved rod measuring about 1.5–5 μm in length and 0.3–0.5 μm in diameter, having 4–6 unipolar, polytrichous flagella. Injury to the gastric mucosa causes epithelial cell damage and regeneration. Arange of histological patterns is recognized
including chronic gastritis, mucosal atrophy, intestinal metaplasia, epithelial dysplasia, and carcinoma.[1,3] The most common cause of intestinal metaplasia is H. pylori associated chronic gastritis.[4] The reported prevalence of H. pylori in patients with chronic gastritis and functional dyspepsia ranges from 39% to 87%.[5-7] It is also associated with gastric adenocarcinoma and lymphoma.[8]
This study was carried out to analyze the histological patterns in gastric mucosal biopsies done for dyspepsia cases.
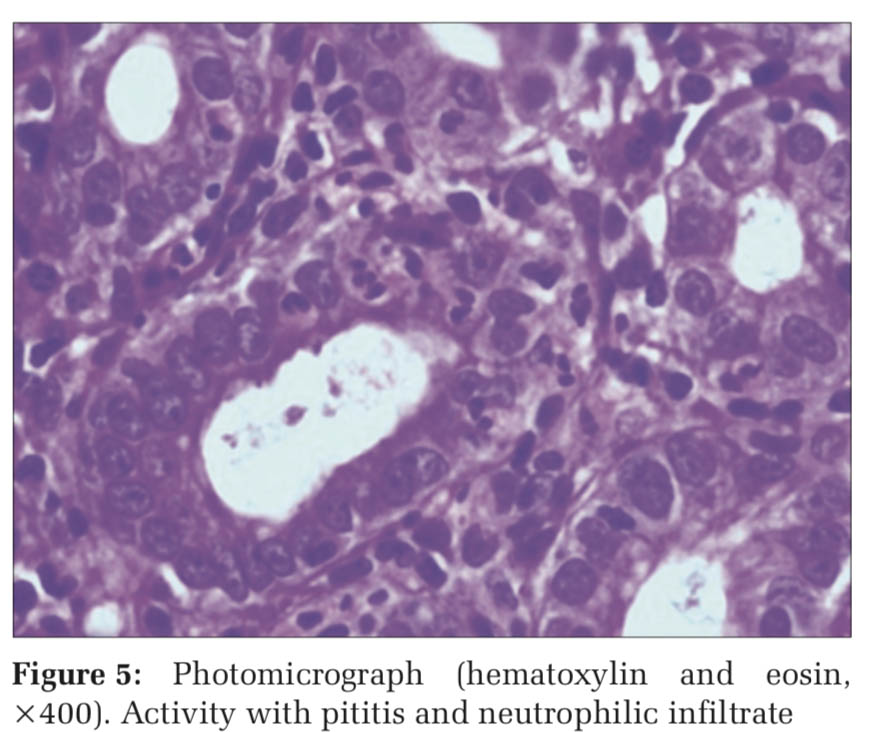
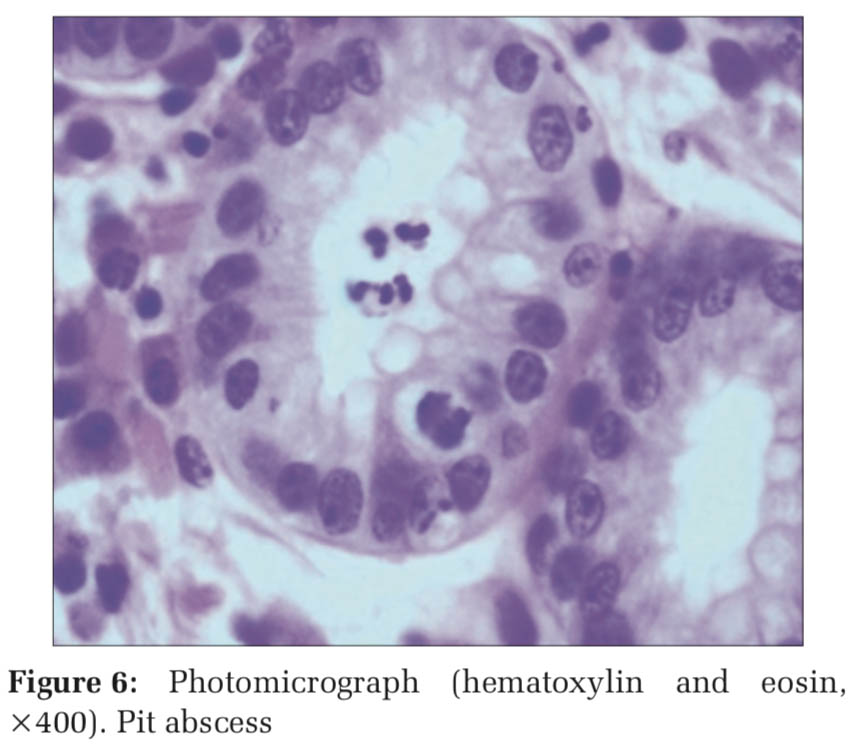
A retrospective morphologic descriptive study over a period of 1 year was done on a total of 550 gastric biopsy samples. The samples from patients with a clinical history of dyspepsia which were received at the department of histopathology were analyzed. The biopsy samples were procured in Bouin’s fixative and were paraffin embedded. Sections were taken and stained with hematoxylin and eosin (H and E). May-Grunwald-Giemsa stain was used to visualize H. pylori. Alcian blue stain was used to identify intestinal metaplasia. “Chronic gastritis” was defined as the presence of infiltration of the superficial and or deep lamina propria by lymphocytes and plasma cells. “Activity” was defined as the additional presence of neutrophils, pititis, and pit abscess. The histological variables of chronic inflammation, activity, intestinal metaplasia, and H. pylori colonization were graded as mild, moderate, and severe.[7]
Chronic inflammation was graded as follows:
Degree of activity was graded as follows:
Intestinal metaplasia was graded as follows:
The colonization of H. pylori was graded as follows:
Atrophic mucosal changes were also looked for.
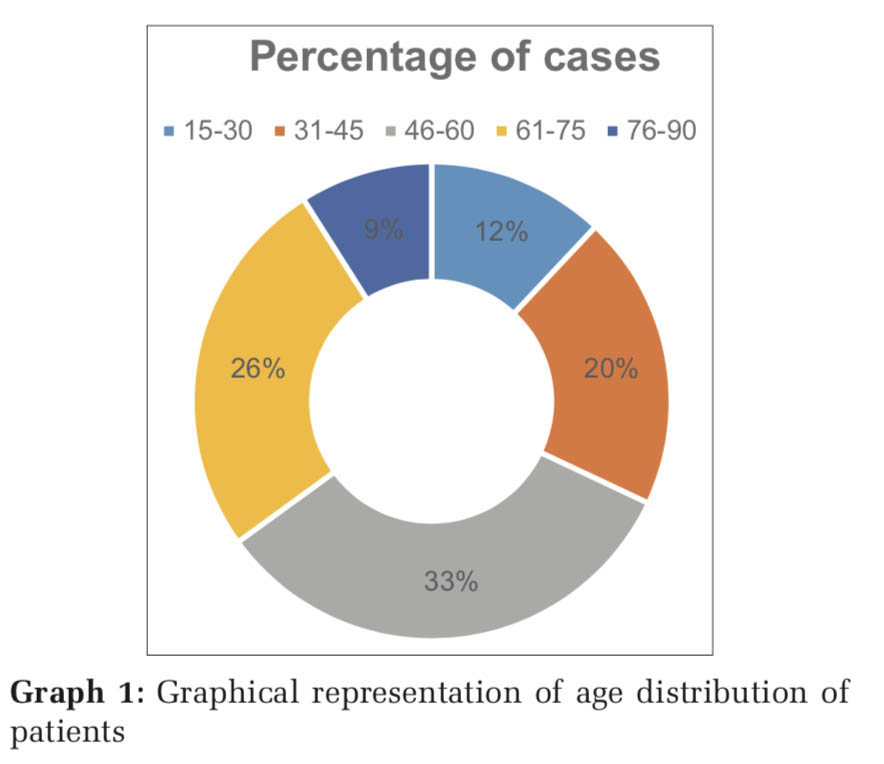
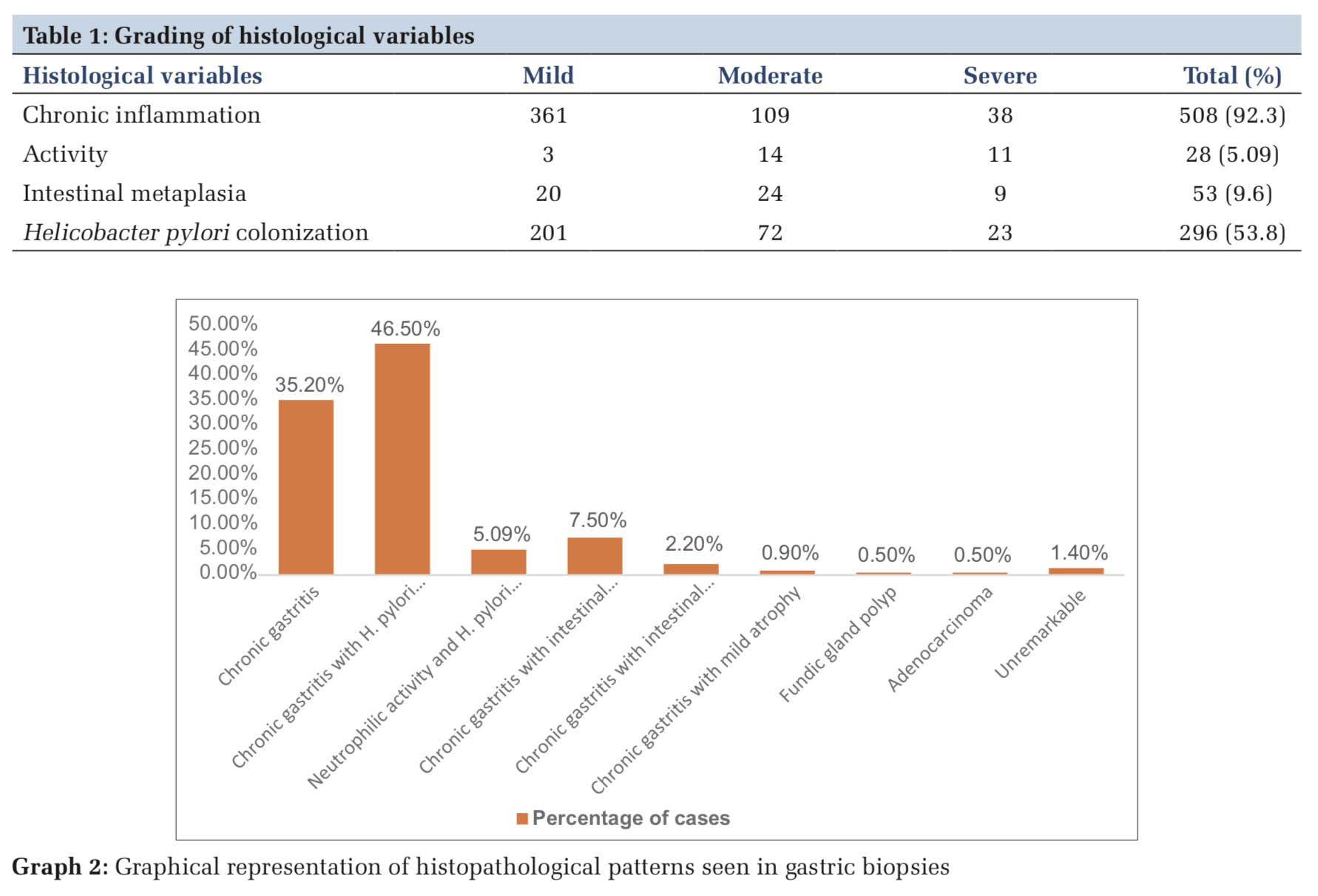
Majority of the biopsies (90%) were from gastric antrum. Of 550 biopsy samples examined, 62% were from male patients, and 38% were from female patients. The males were affected 1.6 times more than females. It was noted that 33% of the patients were between 46 and 60 years of age and 20% were in the age group of 31–45 years (Graph 1). Histopathological patterns were analyzed (Graph 2).
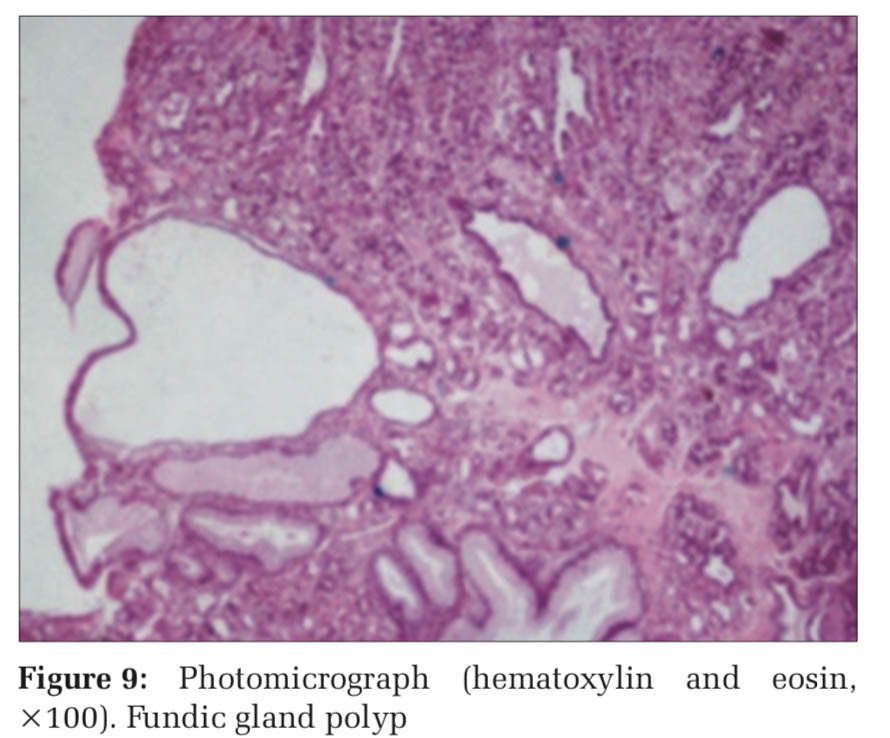
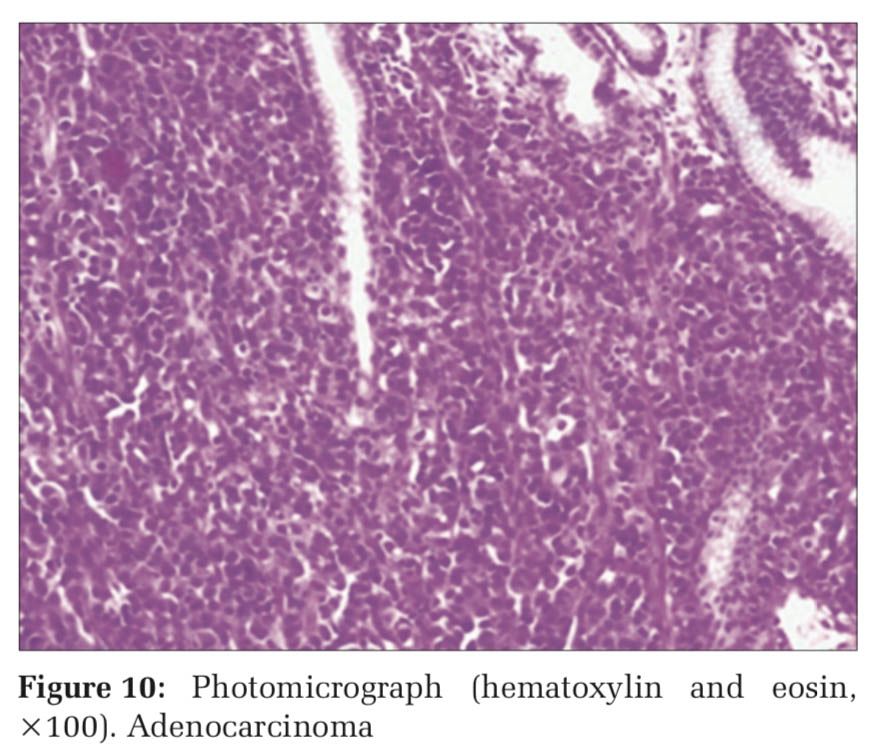
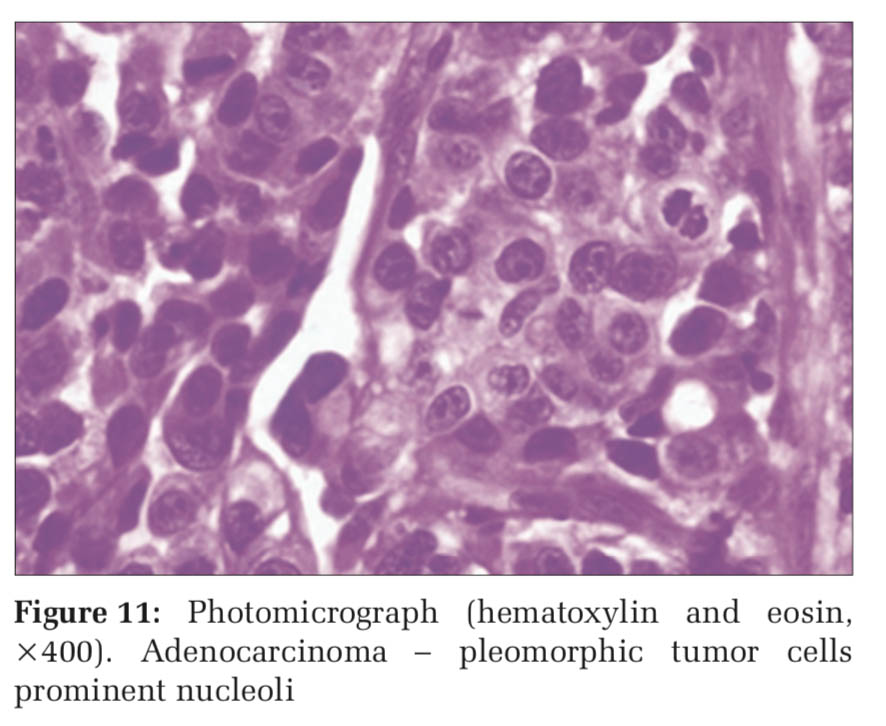
One hundred ninety-four (35.2%) cases showed nonspecific chronic gastritis without H. pylori infection (Figures 1 and 2). H. pylori was noted in a total of 296 cases (53.8%) (Figures 3 and 4) of which 256 cases (46.5%) showed chronic gastritis, 28 cases (5.09%) showed activity with neutrophilic infiltration (Figures 5 and 6), and 12 cases (2.2%) showed chronic gastritis with foci of intestinal metaplasia (Figures 7 and 8). Chronic gastritis with intestinal metaplasia but without any evidence of H. pylori infection was seen in 41 (7.5%) cases. Five cases (0.9%) showed mild atrophy (up to 25% of gastric glands were atrophic). Fundic gland polyp was noted in 3 (0.5%) cases (Figure 9). Adenocarcinoma was diagnosed in 3 (0.5%) cases (Figures 10 and 11).
The histological variables of chronic inflammation, activity, intestinal metaplasia, and H. pylori infection were graded according to severity (Table 1). Of 508 cases showing chronic inflammation, 361 were mild degree showing scattered chronic inflammatory cells, 109 were moderate degree showing focal dense inflammation, and 38 were severe with nearly entire mucosa showing inflammatory infiltrate. Of 28 cases showing activity, 3 cases showed mild Pititis involving 1–2 glands per biopsy. Fourteen cases showed moderate activity involving 25–50% of the glands and 11 cases were graded as severe activity with more than 50% of glands showing pititis and pit abscess. Twenty cases showed mild intestinal metaplasia with involvement of one focal area. Moderate intestinal metaplasia was noted in 24 cases and severe metaplasia involving more than 50% glands was seen in 9 cases. H. pylori colonization was mild in 201 cases where the organism could be identified after careful search. Moderate degree of infection was noted in 72 cases with scattered organisms found at separate foci. Severe infection was noted in 23 cases with numerous H. pylori. The overall percentage of cases associated with H. pylori was 53.8%.
Chronic gastritis is a common condition worldwide. Chronic infection with H. pylori accounts for the Figure11: Photomicrograph (hematoxylin and eosin, ×400). Adenocarcinoma – pleomorphic tumor cells prominent nucleoli majority of cases of chronic gastritis. The basic histological alteration is an increase in the chronic inflammatory cells in the gastric mucosa. The organism interacts with the surface epithelial cells resulting in release of pro-inflammatory mediators, thereby stimulating host non-specific and specific immune responses.[5] Neutrophilic infiltration of the gastric pits and glands is termed as active inflammation. Chronic inflammation shows the presence of lymphocytes, plasma cells, and macrophages.[1] The organism can be demonstrated by H and E stains in biopsy sections, but the sensitivity of the H and E stain is low in tracking H. pylori, probably due to the lack of contrast between the bacteria and the surrounding tissues. In our experience, H and E in combination with a special stain such as Giemsa have been more successful in demonstration of the organism.
H. pylori detection has been aided by invasive and noninvasive diagnostic tests. Serologic test for antibodies, fecal bacteria detection, and urea breath test are few noninvasive tests available.[1]
In the present study, majority of the patients were males (62%). Other authors have also reported gender ratio favoring males. The most likely reason for this observation may be that males are more exposed to risk factors for gastritis and the overall number of male patients attending the outpatient department is higher than females. About 33% of the patients with symptoms of dyspepsia were in the age group of 46–60 in our study.
A high rate of H. pylori associated gastritis (54.2%) has been observed. The results of this study are in agreement with other studies.[1,7,9]
Majority of the cases (92.3%) also showed evidence of chronic inflammation among which 71% of cases were associated mild inflammation. Intestinal metaplasia was seen in 9.7% of cases. The findings are similar to the study conducted by Sharma et al. who reported chronic inflammation in 100% of cases and intestinal metaplasia in 7.8% of cases.[5]
The activity was seen in 28 (5.09%) cases. Mild atrophy was noted in 2 cases (0.3%). These findings are similar to the study done by Sarfraz et al.[6]
Three cases were diagnosed as gastric adenocarcinoma, but there was no evidence of H. pylori infection in these cases. Environmental agents play a role in gastric carcinogenesis.[1]
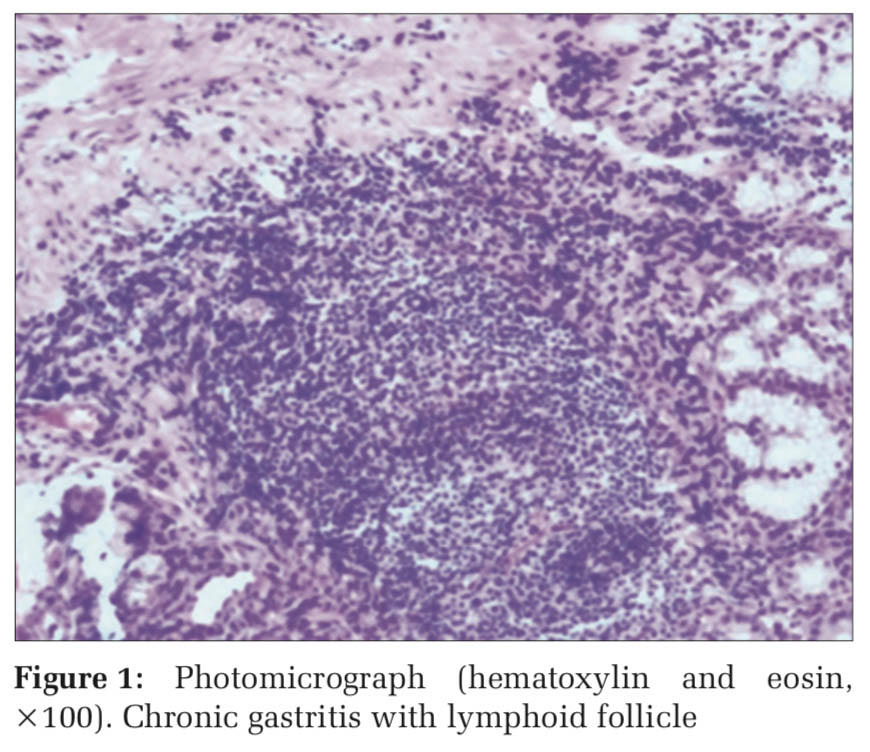
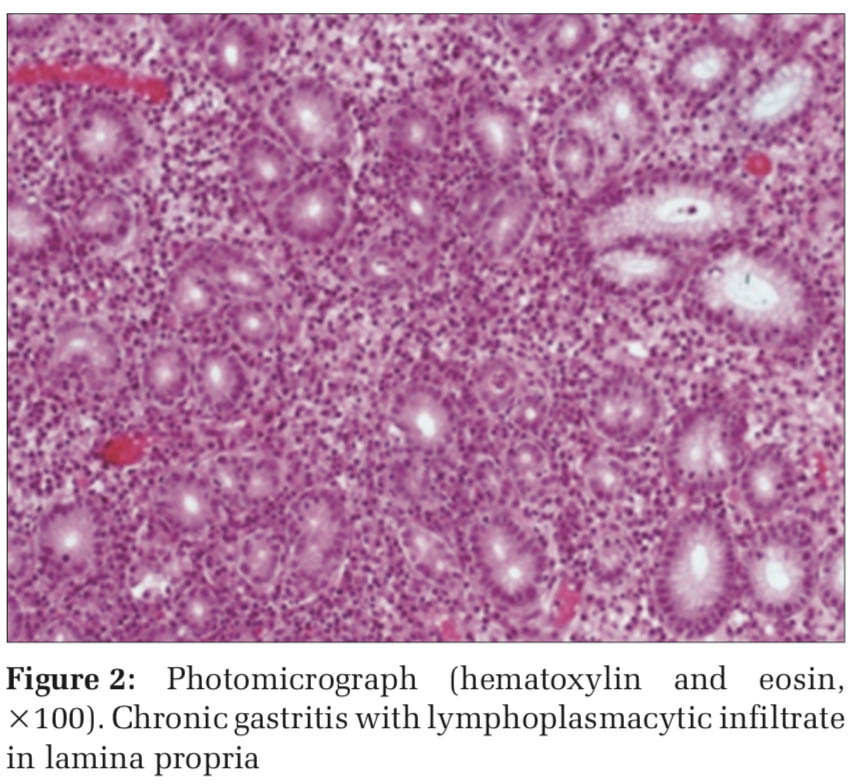
The present study showed a high rate of H. pylori infection in patients with gastritis. H. pylori-induced gastritis shows increased neutrophilic activity along with mononuclear inflammatory infiltrate and presence of lymphoid follicles. Intestinal metaplasia and atrophy indicate the chronicity of the disease.
Subscribe now for latest articles and news.