

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2020.v06i01.006
Year: 2020, Volume: 6, Issue: 1, Pages: 27-29
Case Report
M Gurudutt Kamath1, Madhurima K Nayak2
1Professor, Department of Ophthalmology, Professor, Kasturba Medical College, Manipal Academy of Higher Education, Mangaluru, Karnataka, India,
2 Consultant Ophthalmologist, Department ofOphthalmology Yenepoya Specialty Hospital, Kodialbail, Mangaluru, Karnataka, India
Address for correspondence:
Dr. Madhurima K Nayak, B9, KMC Staff Quarters, Light House Hill Road, Mangaluru - 575 001, Mangaluru, Karnataka, India. Phone: +91-9844885291. E-mail: [email protected]
Ocular involvement in disseminated malignancies can present due to many reasons, most important being direct ocular infiltration by cancer cells. We present a case of choroidal metastatses. A 50-year-old female presented with sudden diminution of vision in the left associated with RAPD and deep episcleral congestion. Fundus examination revealed a solid retinal detachment and was confirmed by B-scan. Fine- needle aspiration cytology of the lymph node and retinal biopsy confirmed the features of adenocarcinoma breast. The past history confirmed the history of mastectomy and chemotherapy. She was later refereed for radiotherapy.
KEY WORDS: Adenocarcinoma breast, choroid, lymph nodes, mastectomy, solid retinal detachment.
Despite recent advances in early diagnosis and effective treatment, an estimated one-third of diagnosed patients will develop metastatic disease.[1] Metastatic tumor accounts for the most common ocular malignancy. The incidence of ocular breast cancer metastatic disease is 5–30%.[2,3] Despite being the most common intraocular tumor, they are rarely seen while the patient is alive. Majority of ocular metastatic sites are created by hematogenous spread, uveal tissue, especially the choroid, being the primary ocular site of metastases. Uveal metastasis can even mimic anterior scleritis.[4] Here, we report a case of metastatic breast carcinoma presenting as retinal detachment.
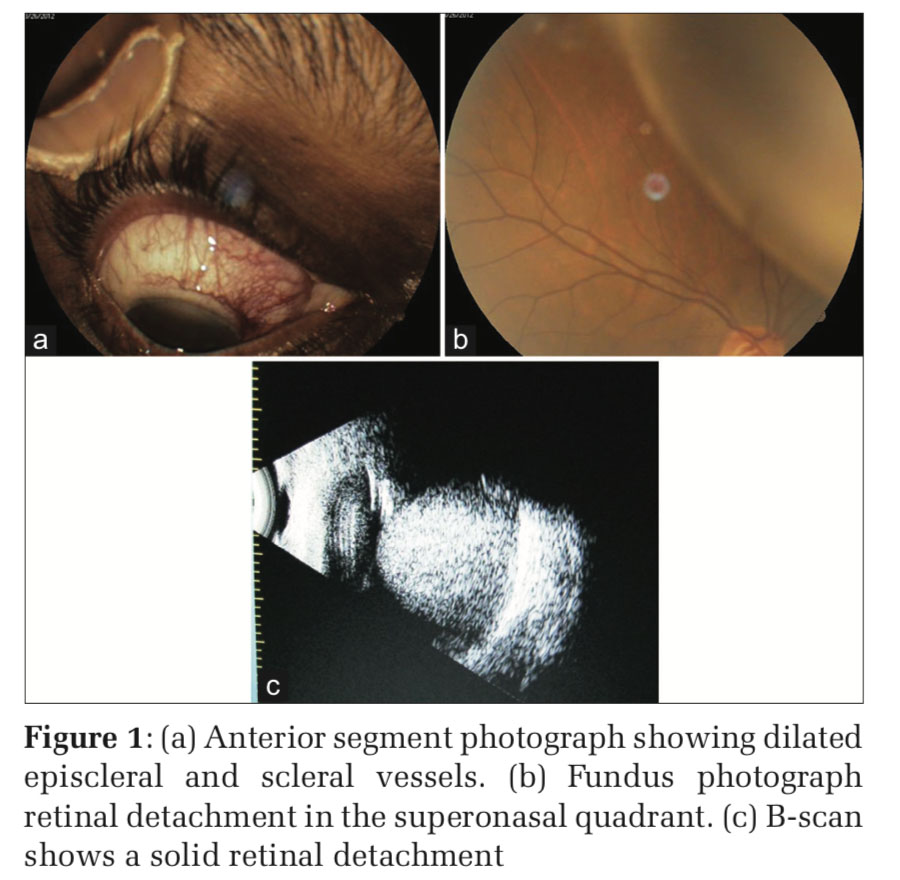
A 50-year-old female presented with sudden diminution of vision in the right eye of 20 days duration associated with pain and redness. The best-corrected visual acuity in the right eye was 6/12, N10 and the left eye was 6/9, N8. Anterior segment examination showed localized episcleral and sclera venous dilatation in the upper nasal quadrant (Figure 1a), relative afferent pupil, and an immature cataract in the right eye. Whereas, the left eye had no abnormal findings other than an immature cataract. Intraocular pressure was 16 mmHg in both eyes. Fundus evaluation showed grayish-white elevated exudative retinal detachment present superonasally, 1 disc size away from optic disc obscuring retinal and choroidal vessels (Figure 1b). Fundus was normal in the left eye. B-scan of the right eye confirmed a solid retinal detachment (Figure1c). On further questioning, she gave a positive history of breast cancer for which she had completed chemotherapy 6 years back.
Keeping metastasis in mind, a thorough metastatic workup was done. It included computed tomography of head, cerebrospinal fluid analysis for cytology, ultrasound abdomen, and chest X-ray, all of which showed negative for metastasis. A retinal biopsy was taken from the superonasal quadrant through a sclerostomy under general anesthesia. The biopsy was sent for histopathological investigations. Our provisional diagnosis was metastatic breast carcinoma to the choroid causing a retinal detachment. The other possibilities were primary intraocular malignancies like choroidal melanoma.
Retinal biopsy specimen showed tumor tissue composed of cells arranged in small loosely cohesive nests and syncytial pattern with scant cytoplasm, pleomorphic nuclei, with large nucleoli (Figure 2a). Immunohistochemistry was negative for estrogen receptors/progesterone receptors (Figure 2b). Ahistory of adenocarcinoma breast treated with modified radical mastectomy and chemotherapy 6 years back and features of retinal biopsy malignancy were suggestive of a pleomorphic variant of lobular carcinoma. The patient was further referred to radiotherapy; however, the patient was later lost to follow up.
Uvea is the most common site of ocular metastasis, choroid being the most common among iris, ciliary body, and choroid.[2] About 5% of disseminated breast cancer patients have been found to have asymptomatic choroidal metastasis.[3] Choroidal metastasis typically appear as yellow plateau- shaped elevations with subretinal fluid.[2] In this case, there was solid mass causing a retinal detachment without affecting the central vision. An adjoining a scan would be helpful to differentiate hemorrhagic and exudative detachment. As we lacked the necessary equipment, it was not possible to perform. On ultrasonography, choroidal metastases usually have irregular bumpy surface and medium to high reflectivity on A scan.[5]
The median interval of appearance of choroidal metastasis following breast cancer is found to be 3 years,[6] while our patient presented 6 years following appearance of primary tumor. Radiation therapy has been found to stabilize and improve vision in such cases[6] and has been found to have 80% response rate.[7]
Choroidal metastasis occurs in up to 10% of systemic metastatic disease and 49.1% of metastasis to eye are from breast cancer.[1] About 30–90% of cases of leukemia have been associated with ocular disorders.[8-10]

Choroid is a common site for metastasis for hematogenously spreading malignancies. This case provides testimony to the fact that choroidal metastasis can be an initial presentation for a distant malignancy. It warrants thorough work up and investigation to find the primary and other sites of metastasis.
Subscribe now for latest articles and news.