

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2020.v06i01.008
Year: 2020, Volume: 6, Issue: 1, Pages: 33-36
Case Report
R Praveen1, M Venugopal2, Simi fabian2, Viji Praveen2
1Consultant Gynecologist Department of Gynaecological Endoscopy, West Fort Hospital, Aswini Hospital and ARMC IVF Fertility Centre, Thrissur, Kerala, India,
2Infertility Specialist Department of Reproductive Medicine, ARMC IVF Fertility Centre, Thrissur, Kerala
Address for correspondence:
Dr. R Praveen, Sukriti, Sree Kerala Varma College Road, Chungam, Ayyanthole, Thrissur - 680 003, Kerala, India. Phone: 8089333651. E-mail: [email protected]
Background: Embryological maldevelopment of the Mullerian or paramesonephric duct results in congenital uterine anomalies. A rare developmental anomaly is a septate uterus with cervical duplication and a longitudinal vaginal septum. This anomaly cannot be explained by the classical unidirectional Mullerian developmental theory and does not fit into American Society for Reproductive Medicine (ASRM) classification of uterine anomalies. The bidirectional Mullerian developmental theory holds good for this type of anomalies and the new ESHRE/ESGE classification for female urogenital tract anomaly (CONUTA) is more suitable for effective categorization, diagnosis, and treatment.
Case Report: Two cases of the complete uterine septum with double cervix and longitudinal vaginal septum who presented with dysmenorrhea, dyspareunia, and infertility were diagnosed and managed by hysteroscopy and laparoscopy. The vaginal and the uterine septum were resected. Both the patients had an uneventful post-operative recovery period and were followed up for a period of 1 year. The symptoms such as dysmenorrhea and dyspareunia improved significantly without any effect on the fertility outcome.
Conclusion:Very few of such cases are reported in the literature. This rare anomaly is explained by the bidirectional Mullerian developmental theory and the application of the new ESHRE/ESGE classification of the urogenital tract (CONUTA) is more suitable for such anomalies for effective categorization, diagnosis, and treatment..
KEY WORDS: Congenital uterine anomalies, double cervix, infertility, longitudinal vaginal septum, medical subject headings, septate uterus.
Studies have shown the prevalence of congenital uterine anomalies to be 2.4% in the general population, 5.6% in the infertility group, and 7.1% in those with recurrent pregnancy loss.[1] The patients may be asymptomatic or present with pelvic pain, dysmenorrhea, pelvic mass, amenorrhea, poor obstetric outcome, or infertility.[1] Septate uterus is the most common anomaly.[2] We report two cases of a rare anomaly, i.e., longitudinal vaginal septum, double cervix, and uterine septum.
Case 1
A 30-year aged lady came with a 2-year history of secondary infertility. She was married for 3 years and had a spontaneous abortion at 3months gestation during her 1st year of marriage. She had regular normal menses with dyspareunia. She was a homemaker and had no medical illness. She had an old ultrasonography (USG) report which showed a double uterus/septate uterus. Neither her siblings nor her mother had uterine anomalies.
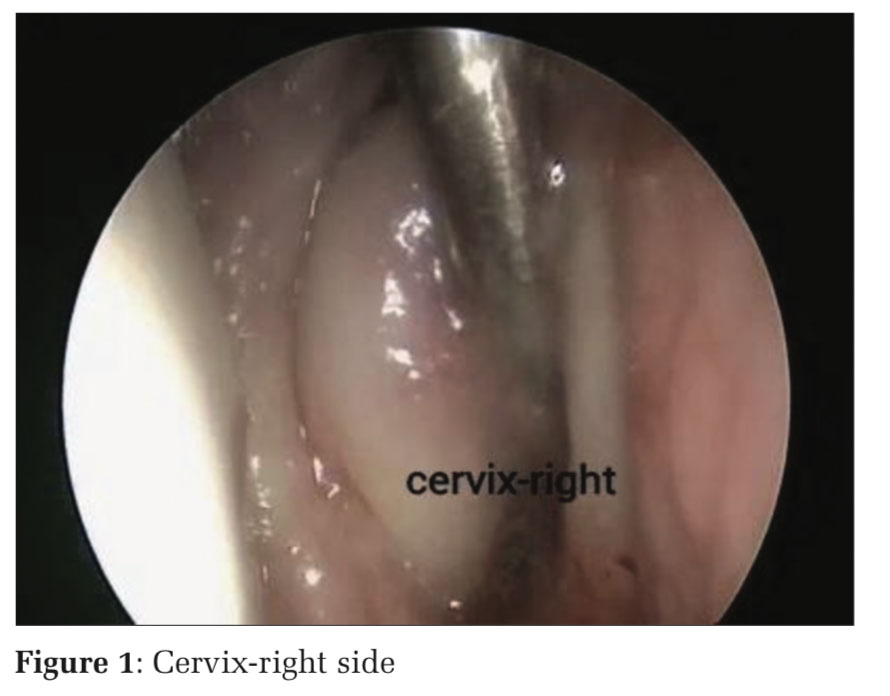
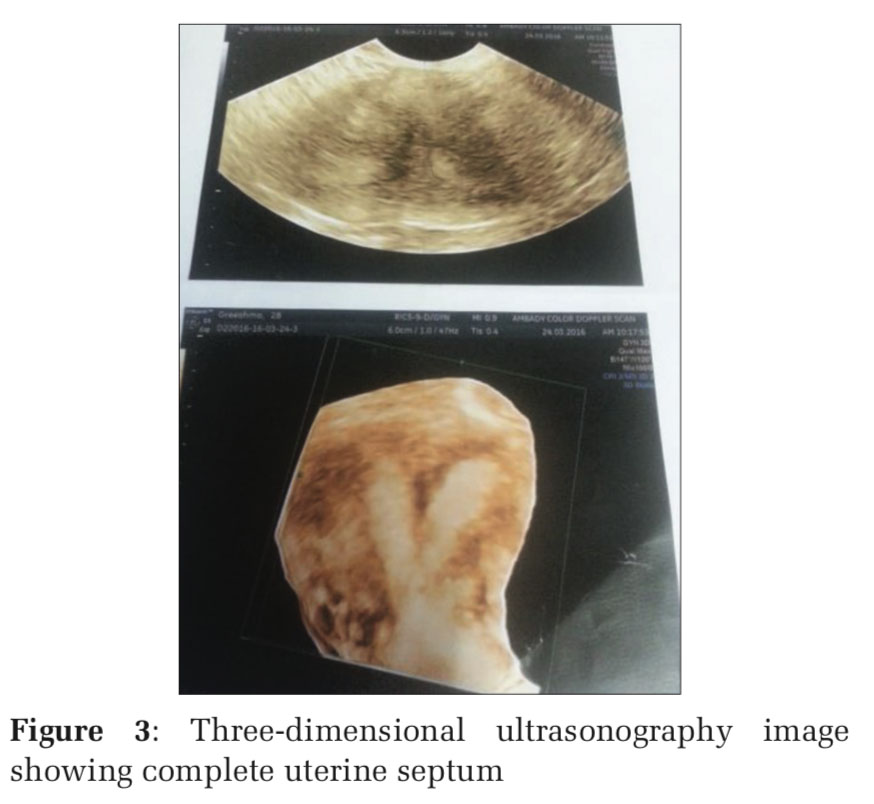
On clinical examination, she had a longitudinal vaginal septum and double cervix (Figures 1 and 2). Three-dimensional (3D) USG confirmed the presence of uterine septum (Figure 3). This patient underwent hysterolaparoscopy under general anesthesia. Longitudinal vaginal septum was resected with monopolar diathermy. Double cervix was confirmed as two separate cervical rings were visible.
Hysteroscopy revealed normal cervical architecture on the intervening tissue between the two cervical canals. Complete uterine septum was visualized with ostia on each side. Laparoscopy showed flat and broad uterine fundus. Uterine septum was resected hysteroscopically above the level of internal os without damaging the intervening tissue between the two cervical canals with monopolar diathermy using a resectoscope with 1.5% glycine as distension medium (Figure 4). Intrauterine 10 Fr Foley’s catheter (3–4 ml NS) was placed for 7 days under antibiotic coverage. The patient was put on conjugated equine estrogen (0.625mg t.i.d) for 12 weeks and medroxyprogesterone acetate (10 mg b.i.d) for a week on 4th, 8th, and 12th week. The patient was followed up for a year, during which she underwent four cycles of controlled ovarian hyperstimulation with intrauterine insemination. Dyspareunia resolved completely; however, she did not conceive.
Case 2
A 22-year aged lady presented with primary infertility and dysmenorrhea. She had regular normal menstrual cycles and was married for 5 years. She was a homemaker and had no medical illness.
On clinical examination, longitudinal vaginal septum and double cervix were found. 3D USG showed complete uterine septum. There was no history of uterine anomalies in her mother or siblings. On hysterolaparoscopy, findings were confirmed and corrective procedure was done. Post- operative management was similar to the previous case. The patient was followed up for more than a year, during which dysmenorrhea improved. She was unable to conceive and is considering Assisted Reproductive Technology (ART).
Uterus, cervix and upper part of the vagina are developed from the Mullerian ducts and the lower part of the vagina by the urogenital sinus.[3] Mullerian anomalies can have variations and may pose a challenge to the clinician while diagnosing and offering therapeutic options.
A systematic clinical examination, 3D USG, magnetic resonance imaging (MRI), and laparoscopy combined with hysteroscopy can accurately diagnose most of the anomalies. In addition, MRI allows for the evaluation of the urinary tract, as 30% of these women have associated urinary tract anomalies.[4,10]
Uterine septum, double cervix and longitudinal vaginal septum are a very rare anomaly with only a few reported cases.[5-10] The existence of such an anomaly cannot be explained by the classical unidirectional developmental theory.[11] Bidirectional developmental theory, as suggested by Muller et al., explains that the fusion followed by resorption of paramesonephric ducts could start at the isthmic portion and progress cranially and caudally at the same time.[5,7-10]
Here, septate uterus is the result of resorption failure of the fused Mullerian duct cranial to the isthmic area and double cervix is due to failure of fusion caudal to the isthmic area. Longitudinal vaginal septum is due to a developmental defect of the paramesonephric duct and urogenital sinus. As this Mullerian anomaly is unique in having two uterine cavities, single fundus, double cervices, and longitudinal vaginal septum, most of the cases are wrongly diagnosed as uterine didelphys without proper treatment being offered.
A recent classification system (classification for female urogenital tract anomaly [CONUTA] recommended by ESHRE/ESGE classifies urogenital tract anomalies as uterine, cervical, and vaginal anomalies separately.[12] This system helps in the proper diagnosis of common as well as rare types of anomalies, including their therapeutic options.
According to this system, the diagnosis is termed as U2bC2V1. The surgical correction for such cases is the excision of longitudinal vaginal septum and uterine septum only, without disturbing the intervening cervical tissue. The resection of the cervical tissue for a wrongly diagnosed septated cervix may lead to cervical insufficiency resulting in second-trimester miscarriage, preterm labor, and premature rupture of membranes, and these women need prophylactic cervical cerclage which would be difficult to perform vaginally and abdominal cerclage would be the only option.
Such women with pregnancy failure, dyspareunia, dysmenorrhea, or requiring ART due to other factors would benefit from an accurate diagnosis and appropriate surgical correction.


Clinicians should be aware of the existence of such a rare anomaly. The recent classification (CONUTA) recommended by ESHRE/ESGE should be advocated more frequently in our clinical practice for all the uterine anomalies so that these rare anomalies are accurately diagnosed and managed.
Subscribe now for latest articles and news.