

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2019.v05i03.002
Year: 2019, Volume: 5, Issue: 3, Pages: 7-12
Original Article
T R Manjula1, K Gahana2, R Harsha3
1Professor and Head, Department of Ophthalmology, Mandya Institute of Medical Sciences, Mandya, Karnataka, India,
2Postgraduate student, Department of Ophthalmology, Mandya Institute of Medical Sciences, Mandya, Karnataka, India,
3Postgraduate student, Department of Anesthesiology, ESI Post Graduate Institute of Medical Science and Research, Bengaluru, Karnataka, India
Address for correspondence:
Dr. K Gahana, D/O Krishnegowda H S, Behind Andhra daabha, NH 75, B.G Nagara, Bellur(H), Nagamangala, Mandya, Karnataka, India. Phone: +91-8151949278. E-mail: [email protected]
Objective: The objective of the study was to find the occurrence of meibomian gland dysfunction (MGD) and dry eye disorder in patients with type 2 diabetes mellitus (DM) and to assess the profile of MGD in type 2 DM patients.
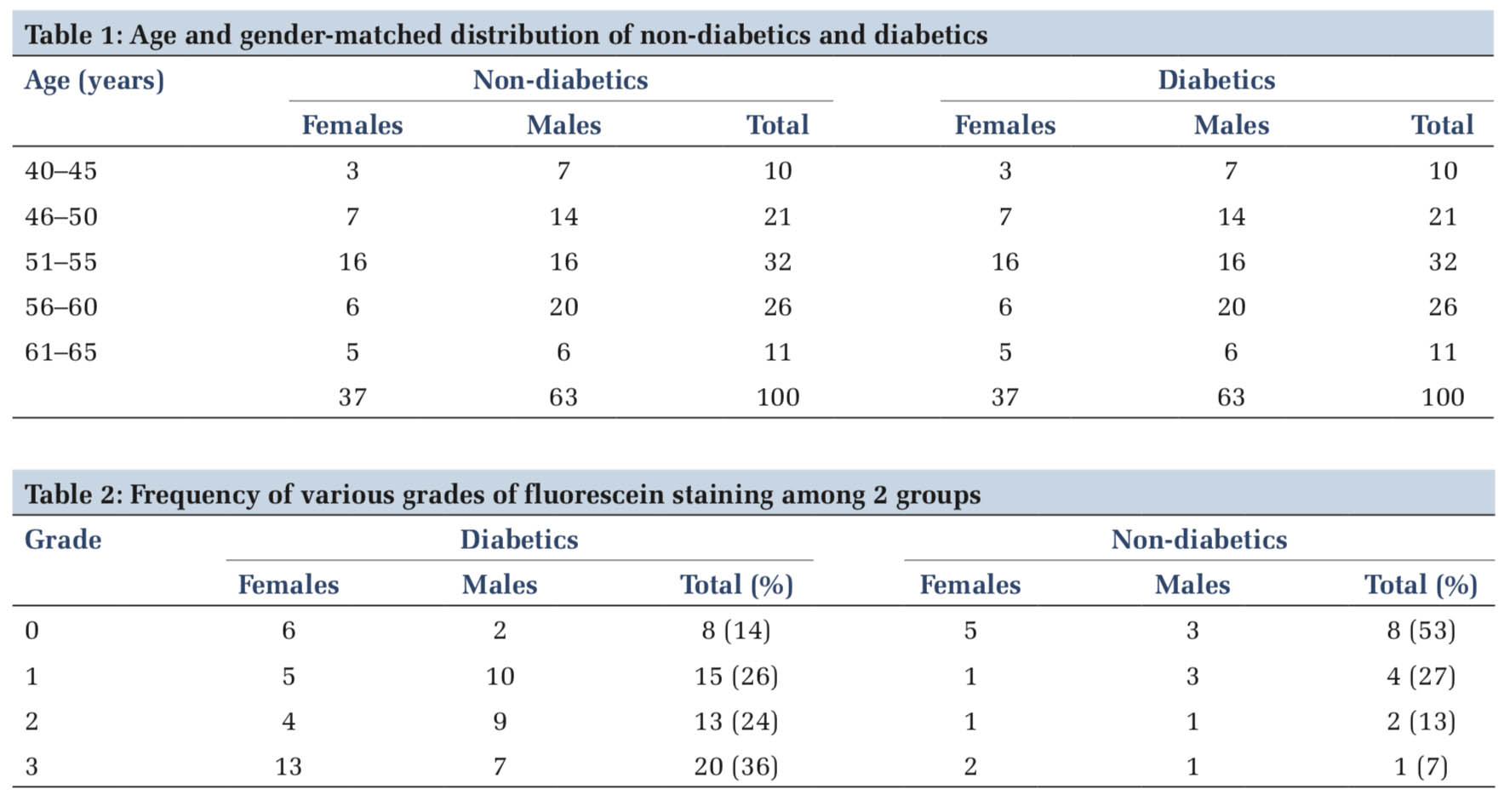
Materials and Methods: An observational case-control study was conducted on 100 type 2 diabetes patients and 100 controls who are attending ophthalmology outpatient department with distinct complaints, for example, correction of refractive error. Age and gender matching was done. Tear film evaluation was done for both the groups, lid margin abnormalities were noted under slit lamp biomicroscope, fluorescein staining of ocular surface performed, and pre-corneal tear film was observed for debris. Schirmer’s test as well as tear breakup time test was performed.
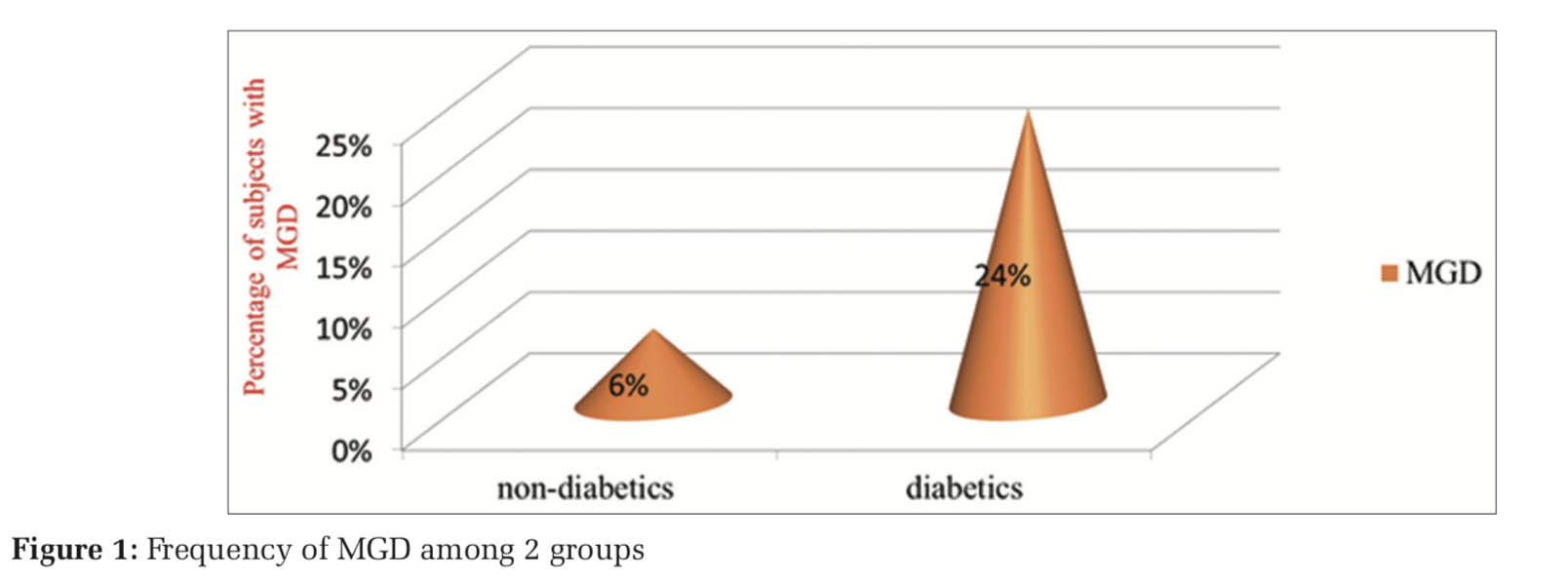
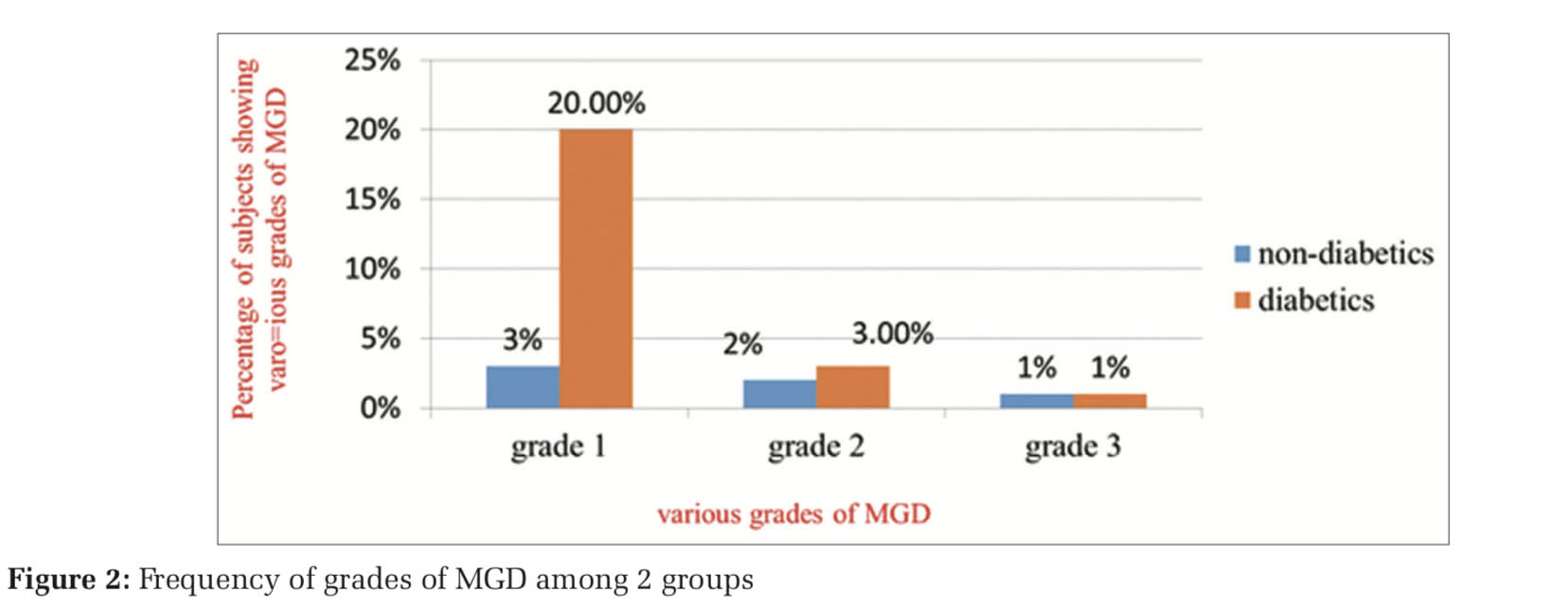
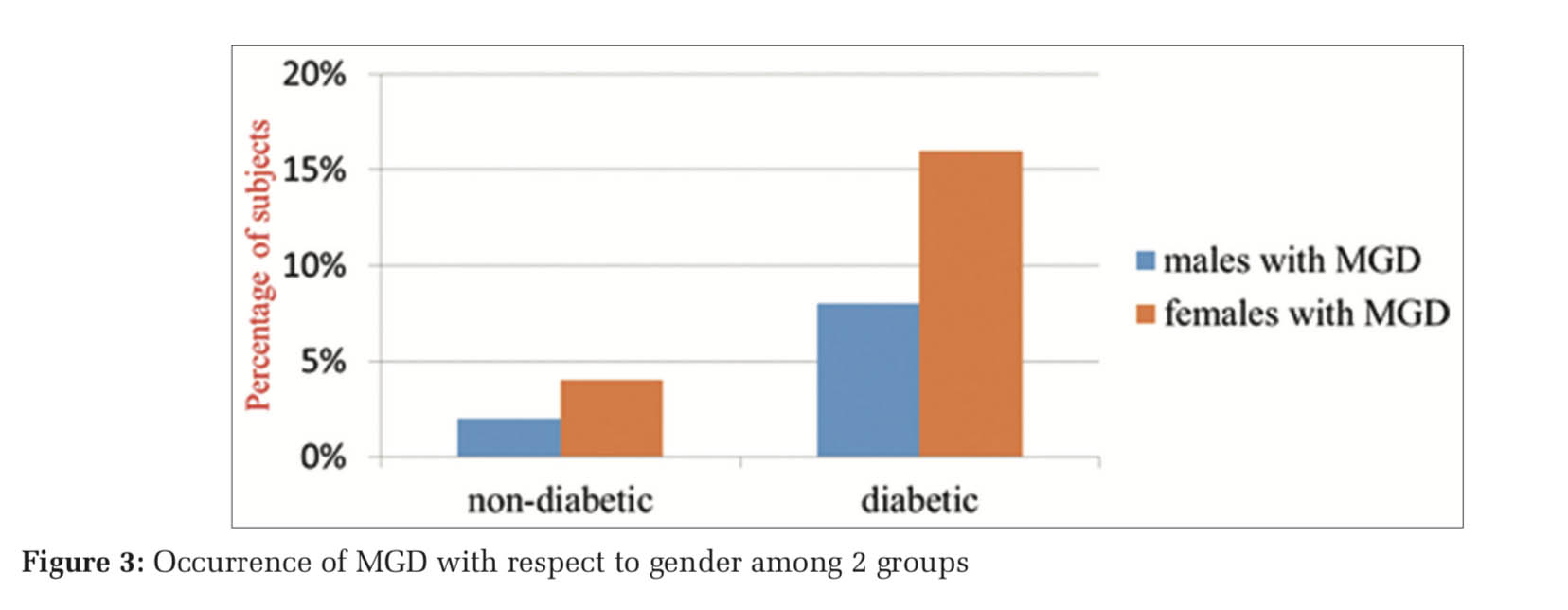
Results: Of 100 diabetic patients, dry eye disorder was found in 56 (56%) cases, among which 24 patients had MGD. Twenty-four of 56 that is 42% of dry eye is credited to MGD. Of 100 non-diabetics, 15% had dry eye disorder, among which 6 cases had MGD.
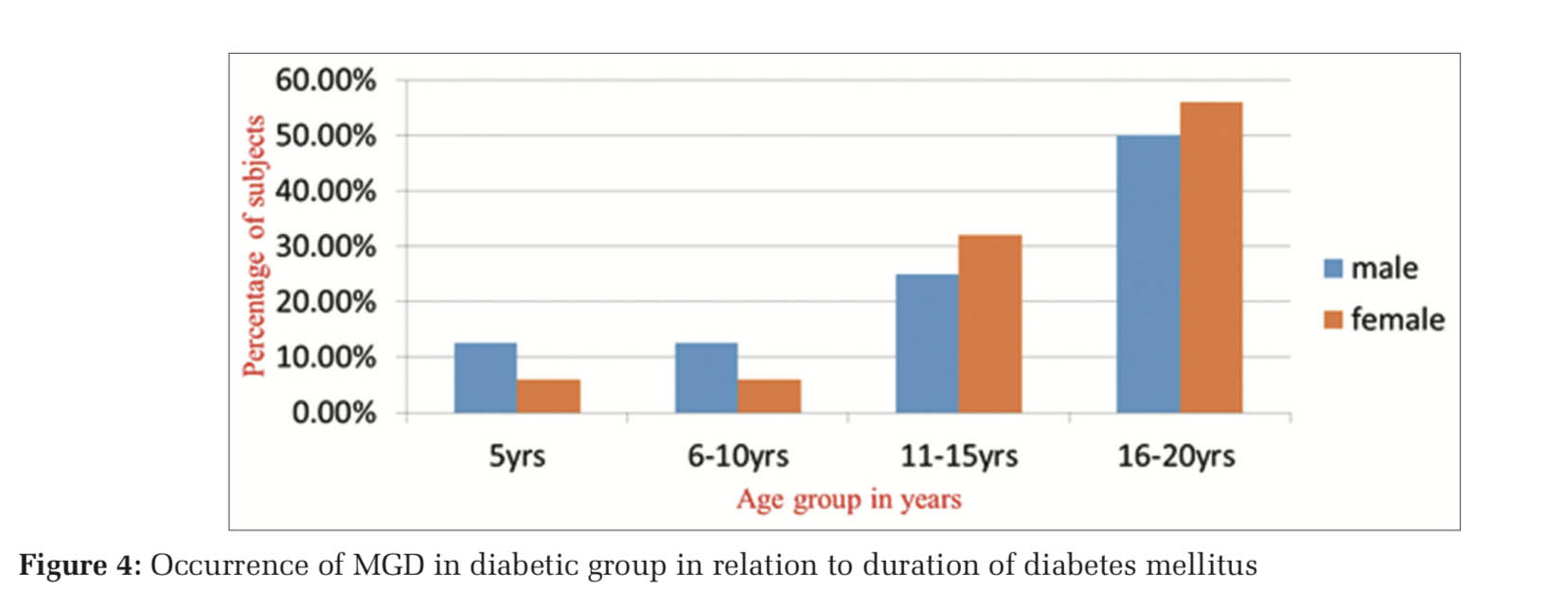
Conclusions: Diabetes can cause changes in ocular surface with respect to both qualitative and quantitative parameters. Diabetic patients are more susceptible for dry eye disorders when compared to normal subjects. In diabetics, the frequency of MGD is considerably more when compared to nondiabetic group. As the duration of DM increases prevalence and severity of MGD also increases proportionately.
KEY WORDS:Dry eye, meibomian gland dysfunction, Schirmer’s test, tear film breakup time.
Diabetes mellitus (DM) is defined as a primary disorder of carbohydrate metabolism, secondarily involving the protein and fat metabolism characterized by glycosuria and hyperglycemia.[1] Diabetes affects various organs and of these perhaps, one of the most important is its ocular manifestations. The incidence of DM is hastily increasing in India, diabetes will perhaps appear as one of the foremost cause of ocular disorder by the time we accomplish something in preventing a larger amount of preventable blindness.[2]
DM is found to be associated with several ocular conditions such as acute orbital infection, hordeolum, variations in the refractive error, chronic inflammation of the lid, neovascular glaucoma, ptosis, diabetic retinopathy, and oculomotor nerve palsies, cataract. Deficiency of tear secretion and dysfunction of tear film for chronic period has also been identified in diabetic patients.[3] Studies have proved that deficient production and secretion of tears is due to “autonomic neuropathy,” in turn causing disturbance to the nerves that supply the lacrimal gland causes dry eye in majority of the cases of dry eye in association with diabetes.[4]
For dry eye disorders, DM is noted as one among the foremost systemic risk factors.[5] Patients diabetic might show symptoms of dry eye due to abnormal lacrimal secretions, metabolic dysfunction, or neuropathy. International Workshop on meibomian gland dysfunction (MGD) tells that MGD might play a significant task in aqueous-deficient dry eye and it is the most prevalent cause of evaporative dry eye.[6] In patients with type 2 diabetes, meibomian gland structure, and dysfunction including meibum expressibility, lid marginabnormalities,andmeibographyscoreswere found to be appreciably inferior.[7]
Diabetes leads to instability in tear film by reducing the number of goblet cells, in turn inducing damage to conjunctival and corneal epithelial, ocular surface hydrophilic environment, and secretion of mucin is also reduced in diabetes.[8,9] A study from Ding et al. established that proliferation of epithelial cells of meibomian gland human meibomian gland epithelial cells is stimulated by insulin, and also showed that high glucose was toxic to these cells.[10] The corneal sensitivity, fluorescein staining score, and the density of corneal epithelial cells and nerve fibers in the diabetic patients show a relationship with the duration of diabetes.[11] Dry eye (keratoconjunctivitis sicca, tear instability) is a disorder of the tear film due to tear deficiency or excessive evaporation and is related to symptoms of discomfort and ocular irritation such as feeling hot, dry, gritty or sandy, burning, smarting sensation, itching, watering, or tearing.[12] The purpose of the study is to evaluate the incidence of dry eye and MGD in type 2 diabetes patients and to compare the results with those of controls.
Clearance from Institutional Ethical Committee in accordance with the guidelines of the Declaration of Helsinki was obtained. Purposive sampling method was used. One hundred cases with type 2 DM and 100 nondiabetic controls, which are matched with respect to age and gender who are seeking medical care for correction of refractive error were enrolled from the ophthalmology department. Informed consent was taken by all study participants.
Inclusion criteria
Exclusion criteria
The following criteria were excluded from the study:
Intestinal metaplasia was graded as follows:
Tear film assessment was done as follows:
A minimum interval of 10 min left between any two tests. All the patients were examined by the same ophthalmologist to avoid interobserver bias. Grading of MGD was done based on guidelines tailored from “The international workshop on meibomian gland dysfunction” Diagnosis of dry eye disorder was made according to the recommendation by TFOS DEWS II report, in which OSDI score of ≥13 and either TBUT <10 s or ocular surface staining showing >5 corneal spots, >9 conjunctival spots, and lid margin (≥2 mm length and ≥25% width) was diagnosed as dry eye.
Data were entered in Excel Sheet using SPSS software Chi-square statistical test was applied to compare the results between two groups.
There is a substantial variation in incidence of MGD in various studies, incidence varies from 3.5% to 70% in relation to different geographic locations.
Kamel et al. showed that in type 2 DM patients and in poorly controlled diabetic patients, there is reduced Schirmer’s I and the TBUT test results (70% in both Schirmer and TBUT).[13] In our study, there is a reduction in the tear film parameter results such as SchT and TBUT in the diabetic patients as compared to controls. This could be due to damage to lacrimal gland microvasculature, causing impaired functioning, moreover, also due to reduced corneal and conjunctival sensitivity in diabetics. One more important contributor is mucin layer of the tear film, which plays integral role in wetting and spreading of tear film, deficiency of which may reduce TBUT value tear film stability, especially in diabetic patients.
Quality and quantity of the meibomian gland secretion, nature of expressibility, and corneal staining are the key parameters used to grade MGD in our study. Evaporative dry eye can be caused by the qualitative and quantitative alterations in the lipid layer, caused by dysfunction in meibomian glands.
Devi and Gowda in their study found that patients aged 50 years (53.6%) showed maximum prevalence rate of dry eye, most of the type II patients, that is, 48.8% of cases were lying in age group between 51 and 60 years.[14] The diabetic patients show higher frequency of the more severe form of MGD.
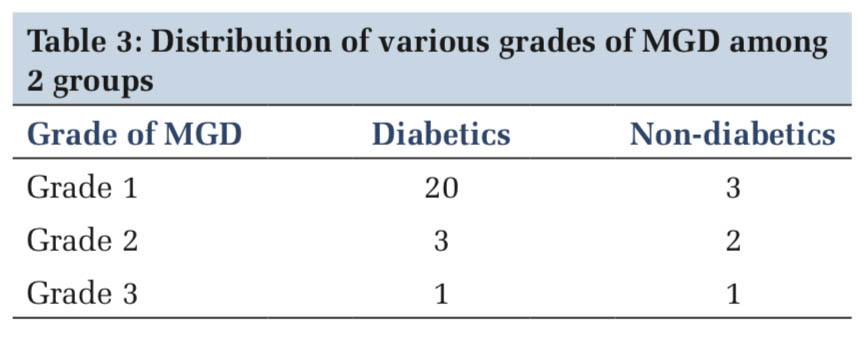
Shamsheer and Arunachalam in their study establish that the diabetic group which comprises 58 eyes showed the highest number of eyes with Grade I–IV lissamine green and fluorescein staining which was a statistically significant difference when compared to the control group with 14 eyes (Chi- square = 32.79, P < 0.0005).[15] In our study, 36% of diabetics with MGD showed Grade 3 fluorescein staining, whereas only 7% of nondiabetic controls showed Grade 3 staining.
A European Community study[16] accomplished that in tear film disorders, objective diagnostic tests and subjective assessments have clinical usefulness as diagnostic tools, aqueous tear disease is interrelated to ocular surface disease.
Moss and Klein[17] in their study reported that diabetic women (16.7%) showed a higher incidence of dry eyes in comparison with males (11.4%). In our study, among the cases with 16–20 years of duration of DM, 56% of female and 50% of male cases exhibited MGD. Estrogen deficiency leading to deficient tear secretion in postmenopausal women has been hypothesized to explain gender differences. Paradoxically, Schaumberg et al.[18] In their study on hormone replacement therapy and dry eye syndrome, reported that there is an increased risk of dry eye found in women on hormone replacement therapy.
The limitation of the present study is, we have not given special consideration to female cases and controls who had attained menopause, which alone can contribute to dry eye disorder.
Subscribe now for latest articles and news.