Introduction
Oral ulcers are one of the predominant complaints of patients visiting ENT OPD. Worldwide estimated prevalence in general population varies from 4.9% to 64.7%. Aphthous ulcers may affect as many as 25% of the population in the world. The prevalence of oral mucosal lesions in South India was 4.1%. 1 An ulcer is a loss or break in the continuity of surface epithelium or mucous membrane that extends into lamina propria. Ulcers are classified as shor-term ulcers, if the duration is less than 3 weeks and long-term ulcers, if the duration is more than or equal to 3 weeks. The causes of ulcero-membranous lesions in oral cavity and oropharynx are numerous and the condition may be confined to oral cavity and oropharynx or may involve mucous membrane of other parts of the body. The causes may vary from non significant to life threatening diseases also. They may be part of local or systemic diseases.
Spounge defines erosion as a shallow crater in epithelial surface that appears clinically as a very shallow erythematous area and implied only superficial damage. He defines ulcer as a deeper crater that extends through the entire thickness of surface epithelium and involves underlying connective tissue.
Because of the variability with which an individual condition may present, as well as the fact that a variety of diseases may behave in a similar presentation within the oral cavity, the practitioner must approach the diagnosis and treatment in an orderly fashion. 2
Morbidity associated with ulcero-membranous lesions in oral cavity and oropharynx and their effect on the general health of an individual is significant. A change in color, texture, or consistency of the oral mucosa requires an explanation. In some instances, history and clinical presentation yield enough information for definitive diagnosis, but often biopsy with submission of lesioned tissue for histologic evaluation is requisite. It is critical for a clinician to identify common oral mucosal lesions readily and to know when a specific lesion requires histologic diagnosis. 3
Oral ulcers have been an everyday problem to many otolaryngologists, physicians and dental surgeons. Many a times, patients are treated symptomatically without even coming to a definite conclusion of their malady. This study aims to determine the etiology of ulcero-membranous lesions in the oral cavity and oropharynx, assess the proportion of patients presenting with various clinical features, and evaluate the need for different treatment modalities, including medical management, surgical intervention and radiotherapy.
Methods
This study, “Clinico-Pathological Study of Ulcero-Membranous Lesions in the Oral Cavity and Oropharynx in a Tertiary Care Hospital,” was conducted from October 2017 to September 2018. A total of 130 patients attending the ENT outpatient department with ulcero-membranous lesions were included through purposive sampling, while those with traumatic injuries without infection and those unwilling to consent were excluded. Institutional Ethics Committee approval was obtained, and informed consent was secured.
Patient history, including tobacco and alcohol use, sexual activity, prior head and neck malignancies, drug intake, joint pain, and family history of skin disorders, was documented. Clinical symptoms ranged from burning sensation and throat pain to dysphagia, odynophagia, halitosis, cough, fever, and weight loss. Systemic cases suggestive of autoimmune disorders or genital ulcers were referred for specialist evaluation. Ulcers were examined for location, size, shape, borders, and fixity. Membranes were assessed for true or false characteristics, while indurated swellings were evaluated for surface texture, tenderness, and bleeding. Neck examination focused on lymphadenopathy.
Diagnostic workup included microbial staining, culture sensitivity, serology (herpes simplex, herpes zoster, p-ANCA, c-ANCA), CBC, and ESR. Biopsy and FNAC were performed for histopathological analysis. Radiological investigations such as CT neck and chest X-ray were conducted in relevant cases. Treatment was planned based on findings.
Results
A total of 41161 patients attended ENT OPD during the study period from October 2017 to September 2018, of which there were 130 patients with ulcero-membranous lesions in oral cavity and oropharynx which accounted to 0.31%. Among these patients 79 were males (60.76%) and 51 were females (39.23%) with male to female ratio of 1.55:1.
The highest number of ulcero-membranous lesions was seen in female patients in the age group 19-40 years (23.85%). Least age of the patient encountered in this study was 5 years in a male child. Highest age of the patient in this study was 80 years. Mean age in this study was 41.24+/-18.39 years.
|
Symptoms |
Number |
Percentage |
|
Odynophagia |
60 |
46.15 |
|
Burning sensation |
57 |
43.83 |
|
Throat pain |
49 |
37.96 |
|
Foreign body sensation |
49 |
37.96 |
|
Dysphagia |
11 |
8.46 |
|
Halitosis |
10 |
7.69 |
|
Swelling in the neck |
08 |
6.15 |
|
Cough |
01 |
0.76 |
*Multiple symptoms were present in the same subject
Most common complaint of oral and oropharyngeal ulcers was odynophagia, followed by burning sensation in throat. Least common symptom was cough (Table 1). All 130 patients presented with throat symptoms whereas 12 patients had associated nasal symptoms, and 11 patients had associated ear complaints.
In our study percentage of patients who had nasal symptoms with a ulcero-membranous lesions in oral cavity were 9.21%. The most common symptom was nasal discharge (6.15%), followed by nasal obstruction and swelling of nose (1.53%). There were no patients who presented with nasal bleed.
In this study group among 130 patients, 47 (36.15%) patients presented with generalized symptoms. Among these, 37 patients presented with fever and 20 patients presented with generalized weakness. 9 patients presented with significant weight loss. Out of these 9 patients with significant weight loss 6 of them found to have malignant ulcers in oral cavity and oropharynx.
In this study group among 130 patients, 18 patients presented with systemic disease like hypertension which accounts about 13.84%. 9 patients had diabetes mellitus, and 3 patients had bronchial asthma. One patient had previous history of pulmonary tuberculosis and had been treated by ATT.
66 patients among 130 study subjects had history of risk factors such as smoking, alcohol, tobacco chewing and exposure to STDs. Among these 66 patients, highest number of patients (51) gave history of smoking. History of alcohol intake was present in 36 patients and 21 patients had history of both smoking and alcohol. 64 patients among 130 subjects did not have any risk factors. Tobacco chewing was present in 14 patients. Out of 27 patients with malignant ulcers smoking history was present in 19 patients, history of alcohol intake was present in 14 patients and history of both smoking and alcohol intake was present in 12 patients.
In our study, the most common etiologic factor for ulceromembranous lesions in oral cavity and oropharynx was infective in nature which accounts for 44.62%. Second most common etiology was inflammatory which accounts to 29.23%.
Thirty nine (30%) patients in our study were bacterial etiology, in that most common bacteria isolated was Enterococcus species. Second most common was Klebsiella and Bacteroides species. In one case acinetobactor was isolated. In two cases viral serology was positive, one was herpes simplex, and another one was herpes zoster. 17 cases were positive for fungus, and all were candida species.
In the study subjects of 130 patients, 38 (29.23%) cases were inflammatory etiology. Among which 7 (5.39%) were RAS- major and 31 (23.84%) were RAS-minor. Among 38 patients with RAS, risk factors like smoking, alcohol and tobacco chewing were seen in 12 patients. One patient with RAS (Minor) had Steven Johnsons syndrome.
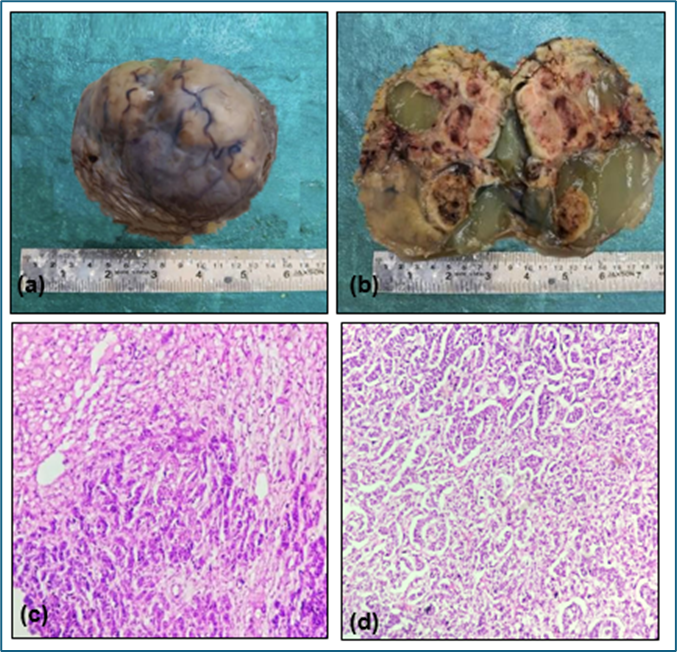
In our study of ulcero-membranous lesions of oral cavity and oropharynx, 27 cases out of 130 study subjects were malignant etiologies. Among 27 malignant ulcers most common location found was tongue followed by soft palate, retromolar trigone and tonsillar fossa.


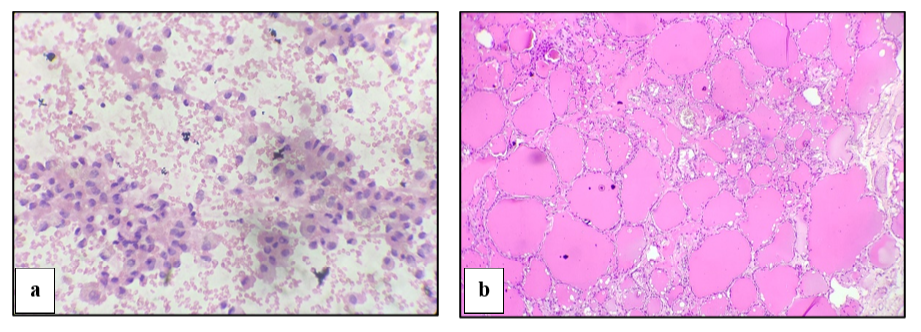
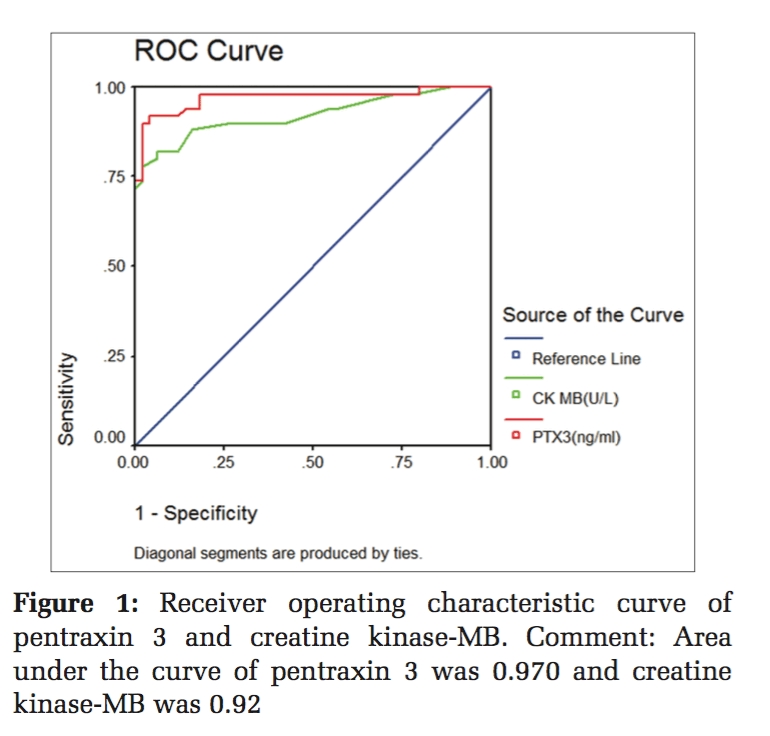
Apart from the above-mentioned etiological factors, various miscellaneous conditions also presented as ulcero-membranous lesions in oral cavity and oropharynx (Figure 1). In this study these conditions were nicotine stomatitis (3), leukoplakia, radiation mucositis, pemphigus vulgaries and oroantral fistula (one each).
102 (78.46%) cases were managed conservatively. Out of 27 patients with malignant ulcers 26(20%) patients opted for radiotherapy and one patient with malignant ulcer on tongue was managed by hemiglossectomy with neck dissection. One more case of oroantral fistula was also treated surgically (Figure 2).
Discussion
Oral mucosal conditions may be caused by local factors (bacterial or viral), systemic diseases, drug-related reactions or lifestyle factors such as the consumption of tobacco, betel-quid and alcohol. Ulcero-membranous lesions in oral cavity and oropharynx accounts to 0.31% of the cases seen in ENT services during the study period.
Male to female ratio of 1.55:1 was seen in our study which is in comparison to study done by Manjunath K which also shows male preponderance. 4
Most commonly affected age group for ulcero-membranous lesions in oral cavity and oropharynx in our study was 19-40 years (42.30%) which is also seen in studies by Manjunath K and Isaac U. 4, 5 The youngest patient encountered in this study was a 5 year old boy and eldest patient was 80 years old male.
In this study 66 patients had history of risk factors like smoking, alcohol consumption, tobacco chewing, exposure to STDs, radiation exposure, prolonged usage of denture. Smoking with alcohol consumption present in 21 patients and smoking, alcohol and tobacco chewing was present in 1 patient. 64 patients did not have any predisposing risk factors for development of ulcers in oral cavity.
All 27 patients who presented with malignant ulcers had history of either tobacco usage (smoking/tobacco chewing) or alcohol consumption for more than 10 years which is in accordance to studies done by Thimmappa TD, Manjunath K, Isaac U, Saintrain MV and Phelan JA. 4, 5, 6, 7, 8
In our study patients presented with odynophagia (46.15%), burning sensation (43.84%), throat pain (37.69%) and foreign body sensation as the most common complaint. In a study by Sridhar RD throat pain was the most common symptom followed by odynophagia which is in contrast to our study.9 10 patients presented with nasal symptoms and 8 patients presented with ear complaints. 57 patients out of 130 presented with generalized symptoms such as fever, malaise, skin lesions, and weight loss.
Associated comorbidities like hypertension, diabetes mellitus, asthma and pulmonary Kochs were present in 35 patients.
Most common etiology for ulcero-membranous lesions in oral cavity and oropharynx was infective (44.62%) followed by inflammatory (29.23%) origin. Study done by Thimmappa TD, Goyal R and Manjunath K shows 50% were of inflammatory etiology which is contrast to our study. 4, 6, 10 Study done by Sridhar RD shows that most common bacteria isolated from ulcero-membranous lesions in oropharynx was diphtheria, followed by streptococcus which is in contrast to our study where Enterococcus sp., followed by Klebsiella, Bacteroides and Haemophilus influenza are the commonly isolated bacteria. 9
Recurrent aphthous stomatitis was found in 38 (29.23%) patients, most commonly in 20-40 age group with male preponderance (M:F-20:18). Of the 38 patients 25 patients didn’t have any predisposing factors. Recurrent aphthous ulcers were the most common entity found in studies by Scully C, Goyal R and Manjunath K which constituted about 50% which is in contrast to our study. 4, 10, 11
In our study malignant ulcers in oral cavity constitute about 20.77% which is similar to studies done by Manjunath K and Mahavar P. 4, 12 Studies by Thimmappa TD shows only 6.5% were malignant which is less compared to our study. 6 The most common site of malignancy in oral cavity and oropharynx in this study was tongue (Figure 3) followed by soft palate and retromolar trigone. Study done by Mathur PT showed that the most common site was buccal mucosa which is in contrast to our study. 13
Malignant ulcers (27 out of 130 subjects) were most commonly seen in the age group of 40 – 80 years in male patients. In this study, male preponderance (23 male patients out of 27 patients with malignant ulcers) was found in patients having malignant ulcers, which is comparable to studies done by Thimmappa TD, Manjunath K and Isaac U. 5, 6 Only 4 female patients were encountered in malignant ulcer group. One study by Saintrain MV showed female preponderance of oral malignant lesions which is in contrast to our study. 7
Miscellaneous causes for ulcero-membranous lesions in oral cavity and oropharynx found in our study were nicotine stomatitis in 3 patients, leukoplakia (Figure 3), Radiation mucositis, pemphigus vulgaris (Figure 3) and oroantral fistula with ulcer in 1 patient each. These are seen most commonly in the age group of 40-70 years with male to female ratio of 1.3:1. This is comparable to the study done by Manjunath K. 4
In our study 102 out of 130 cases were managed conservatively. Patients with recurrent apthous stomatitis were treated symptomatically with multivitamins, antioxidants, antacids, topical anaesthetic agents, and antiseptic gargling solution. 2 patients with viral etiology were treated with oral acyclovir and topical anesthetic agents. 17 patients with oral candidiasis were treated with oral fluconazole, topical clotrimazole and topical antiseptic gargling solution. 26 patients received radiotherapy and about 2 patients underwent surgery. Studies by Thimmappa TD, Goyal R, Scully C and Patil S also shows that majority of them were managed conservatively which is similar to our study. 6, 10, 11, 14

Limitations
-
Relative risk and attributable risk of smoking, tobacco chewing and alcohol consumption for malignant ulcers needs to be calculated in two separate cohort groups with or without malignant ulcers.
-
Long term follow up needs to be done to determine the frequency of recurrence, predisposing factors and evaluation of recurrent aphthous stomatitis.
Conclusion
Our study provides valuable insights into the clinico-pathological profile of ulcero-membranous lesions in the oral cavity and oropharynx in a tertiary care setting. Infectious etiologies emerged as the most common cause, followed by inflammatory conditions. The diverse clinical presentations highlighted the importance of a thorough diagnostic approach to differentiate between benign, infective, and potentially malignant lesions. Conservative management was effective in the majority of cases, emphasizing the role of early diagnosis and appropriate medical therapy in improving patient outcomes.
Declarations
-
Funding: Nil
-
Conflict of interest: Nil
-
Ethical approval: Approved