

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2019.v05i01.001
Year: 2019, Volume: 5, Issue: 1, Pages: 1-6
Original Article
Latesh B Raghute1, Kavita M Jaiswal1, Sujata Dudhgoankar1, Amit Turkar2, Ashutosh Jawade2, Lohit S Vaishnao2
1Department of Pharmacology, Government Medical College, Gondia, Maharashtra, India,
2Government Medical College, Gondia, Maharashtra, India
Address for correspondence:
Dr. Kavita M Jaiswal, Department of Pharmacology, Government Medical College, Gondia, Maharashtra, India.
Phone: +91-9370052826. E-mail: [email protected]
Introduction: The WHO has developed medication use indicators, including prescription indicators with an aim to evaluate the services provided to the population in regard to medications. With the help of these indicators, there will be constant watch on drug prescribing pattern in health care to avoid irrational prescribing.
Objectives: The objective of the study was to find out the rationality of prescriptions by using the WHO core and complementary indicators.
Materials and Methods: This was a cross-sectional study conducted in tertiary care teaching institute over 4 months. The outpatient department prescriptions were assessed for the rationality of the WHO core and complimentary indices.
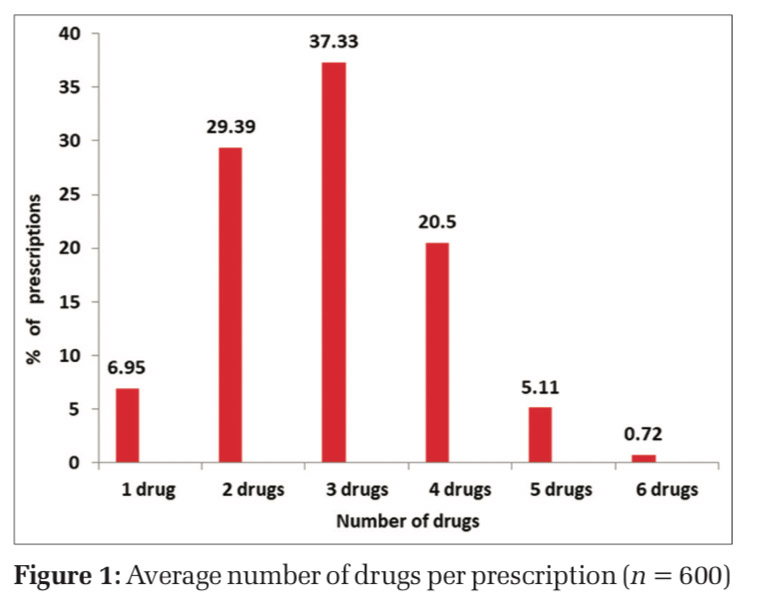
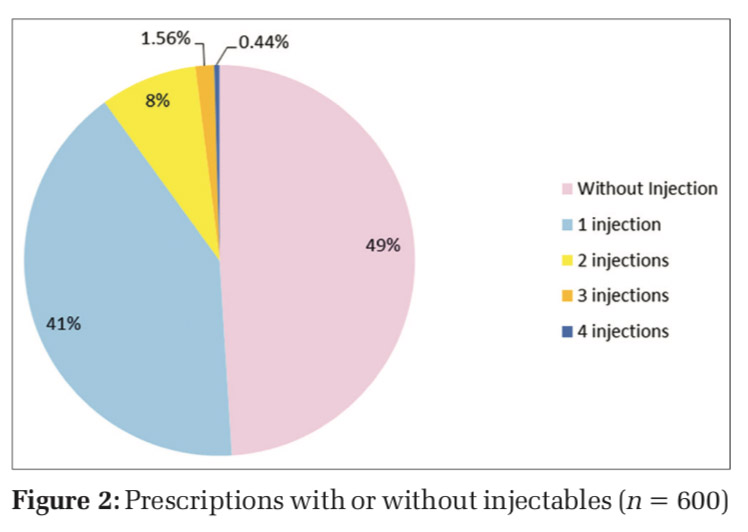
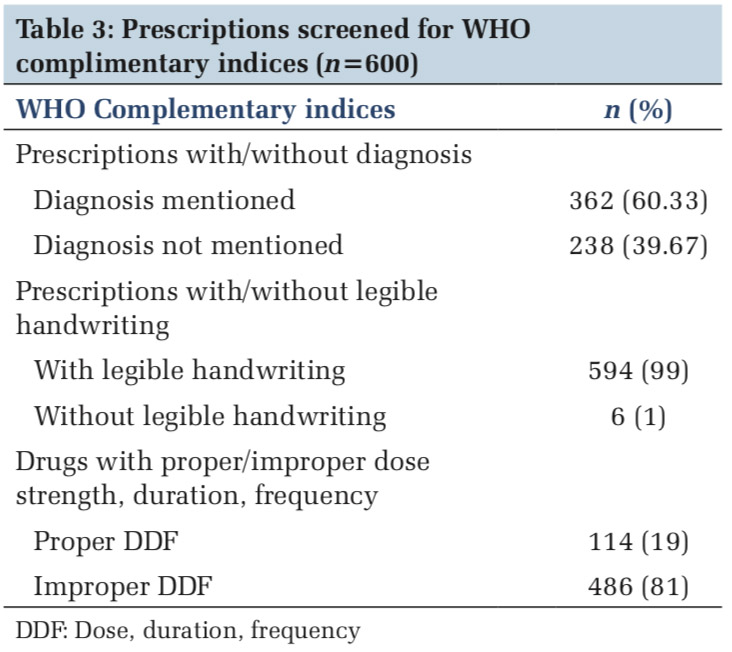
Results: A total of 600 prescriptions were assessed. Prescriptions with the antimicrobial agent were 270 (45%). 1139 (65.69%) drugs were prescribed with generic names while the rest 595 (34.31%) were prescribed by brand names. Prescriptions with banned fixed-dose combinations were 22 (3.67%). A number of medicines prescribed from the national list of essential medicines (NLEM) were 1307 (75.37%) and 427 (24.63%) prescribed were not included in NLEM. The average number of drugs per prescription was 2.89 with a range from 2 to 8 drugs. 246 (41%) prescriptions contain one injectable drug and 48 (8 %) contain two injectable drugs. In 362 (60.33%) prescriptions, diagnosis was mentioned. In maximum prescriptions, 594 (99 %) the handwriting of the prescriber was legible, while in only 114 (19 %) prescriptions proper dose, duration, and frequency (DDF) of drugs prescribed was mentioned.
Conclusions: In the present study prescribing practices for antibiotic and injectable drugs show deviation from the standard recommended by the WHO. Although the handwriting was legible, correct diagnosis, DDF was not mentioned in most of the prescriptions. The prescribers should be given continued medical education and standard treatment guidelines regarding rational prescribing to improve medical services in context to medication.
KEY WORDS:Antibiotics, generics, injectables, rationality.
A prescription is the physicians written order to the pharmacist for dispensing medications.[1] It must be free from ambiguity and should not induce confusion in the patient or the pharmacist. Appropriate prescribing is the outcome of the decision-making process that maximizes net individual health gains within the society’s available resources.[2] Prescription writing is a science and an art, as it conveys the message from the prescriber to the patient. Rational prescription writing is a skill which should be practiced by all prescribers. The treatment of diseases by the use of essential drugs, prescribed by their generic names, has been emphasized by the WHO and the National Health Policy of India.[3] WHO developed medication use indicators, including prescription indicators with an aim to evaluate the services provided to the population in regard to medications.[4] With the help of these indicators, there will be constant watch on drug prescribing pattern in health care to avoid irrational prescribing. Regular assessment of drug prescribing pattern will help us to find out various factors which lead to irrational prescribing, its impact on society and health-care system. This kind of exercise can sensitize prescriber for rational prescribing. Besides, the WHO drug prescribing indicators, there are some complementary indicators to evaluate prescribing practices which varies according to the institute.[4] It mainly depends on local irregularities or mistakes regarding the prescription pattern. The WHO prescription indicators are as follows:
Average number of drugs per medical prescription
This indicator helps in investigating polypharmacy, which is a major factor contributing to adverse drug reactions and drug-drug interactions (DDIs).
Percentage of drugs prescribed by generic name
This indicator helps in controlling drug costs in the health service. It also assesses the prescriber’s influence by drug promotion.
Percentage of drugs prescribed from essential drug list
This indicator helps in controlling the overall cost of medications.
Percentage of prescriptions with an antibiotic
This parameter assesses the excess use of antibiotics which contributes to bacterial resistance.
Percentage of prescribed injectable drugs
This indicator helps to evaluate the unnecessary use of injectables that can cause prick troubles to the patient, necrosis if wrongly administered or sometimes serious complications such as anaphylactic reactions and adverse reactions.
Evaluation of drug use patterns with the WHO drug use indicators has been reported in literature.[5-7] The prescribers are prescribing without keeping in mind the rationality of the WHO core and complementary indices which leads to the irrationality of prescription writing. There should be a chart of the WHO prescribing indices displayed in each outpatient department (OPD) for the prescribers.
Aim and objectives
The present study was carried out:
This cross-sectional study was conducted in the outpatients department of a tertiary care teaching institute of central India for a period of 4 months (January–April 2018). Prior permission was obtained from the Institutional Ethics Committee for conducting the study. Batches of ten 2nd MBBS students of the institute visited the study site thrice a week as a part of their practical learning to collect the data. The motive of involving the students was to teach them the importance of rational use of medicines and prescribing. They were accompanied by a faculty member from the department of pharmacology for the purpose of data collection. Data collection was done by reading and noting down the contents of a prescription. Details of the prescription were entered into a specially designed pro forma [Annexure 1]. The sample of 600 prescriptions was selected. Photographs of the prescription were clicked and saved in the folder for reference. Following information was gathered from the prescriptions- name of OPD, age and gender of the patients, diagnosis mentioned/not mentioned names of drugs prescribed, dose, duration, and frequency (DDF) of medications prescribed, number of antimicrobial agents (AMAs) prescribed per prescription, and number of injectables prescribed per prescription. The following WHO core indices were used to assess the rationality of the prescriptions:[4]
The prescriptions were also screened for complimentary indices such as:
Statistical methods
The sample of 600 prescriptions was selected as per the guidelines given by the WHO for prescription auditing at any hospital set up.[6] Microsoft office (excel) version 2010 and statistical software SPSS version 16.0 (IBM Corporation, New York, United States) were used for collecting, storing, and analyzing data in terms of average and percentages.
During the period of 4months, a total of 600 prescriptions of men and women in all the age group were analyzed. Table 1 shows a number of prescriptions from different OPDs. More than 50% of prescriptions were from medicine OPDs followed by surgery, psychiatry, skin/VD, and others. The most commonly prescribed drugs were paracetamol, diclofenac sodium, cetirizine, and ranitidine. Table 2 shows prescriptions analyzed for the WHO core indices. Maximum prescriptions were without any AMA. Further analysis among prescriptions with AMA use shows, maximum prescriptions were with one AMA. The commonly prescribed antimicrobials were ciprofloxacin, amoxicillin, metronidazole, and Cefixime. A total of 1734 drugs were prescribed; among them the average number of drugs per prescription was 2.89 with a range from 2 to 8 drugs. However, 158 prescriptions (26.33%) out of 600 contain four or more drugs (Figure 1). There were 294 (49 %) of prescriptions with no injectable drugs; however, 246 (41%) prescriptions contain one injectable drug and 48 (8 %) contains two injectable drugs (Figure 2).
Table 3 shows prescriptions screened for the WHO complimentary indices, in maximum prescriptions, the diagnosis was mentioned and was written in legible handwriting, but DDF was proper in very few prescriptions.
In the present study, the average number of drugs per prescription was 2.89 with a range from 2 to 8 drugs, which is higher than the range as compared with the standard (1.6–1.8) derived as ideal[10] and is also higher as compared with the WHO’s recommended value of 1.3–2.0.[11] The same is found to be higher in studies of Uike et al. (4.41), Upadhyay et al. (3.76), and Raj et al. (4.98),[7,12,13] while in a study done by Chandelkar and Rataboli average number of drugs prescribed was found to be 1.8 which falls within the acceptable range.[6] Polypharmacy is defined as the use of five or more medications. In the present study, polypharmacy was found to be in 35 (5.83%) prescriptions. With polypharmacy, there is an increase the chance of DDIs. Practice of polypharmacy by the prescribers may be due to powerful drug promotion and financial inducements by medical representatives. The other reason could be a shortage of the therapeutically correct drug. The percentage of drugs prescribed by generic name in our study is 1139 (65.69%) which is low compared with the standard derived to serve as an ideal (100%).[10] This indicates majority of drugs were prescribed with a generic name, but still there was a big percentage regarding the use of the brand name.[14] This findings corelates with other studies.[6,7,15,16] The benefits of prescribing drugs as generics is that it avoids confusion increases patient’s compliance and lowers cost of therapy. The reasons for high prescriptions of nongenerics could be again the influence of doctors by pharmaceutical companies. In the present study, the total percentage of encounters with antibiotics was 45%, whereas with the WHO standard guidelines it is < 30%. Empirical use antimicrobial susceptibility testing prevents the misuse of antibiotics and thus resistance problem is taken care of. The most commonly prescribed antibiotics were ciprofloxacin (11%), amoxicillin (9%), metronidazole (3%), ceftriaxone (3%), and cefixime (3%). In this study about, 49% of prescriptions were found to be prescribed with no injectable drugs whereas 41% of prescriptions contain one injectable drug and 10% contains more than 2 injectable drugs, and the rest 12 (2%) were with more than 2 injectables; hence, the total prescriptions with injectable drug were found to 51% which is very high compared to the standard (13.4%–24.1%) derived to be ideal.[10] Prescriptions with more number of injectables have been reported in various studies conducted by different authors.[7,17-19]
Possible reasons for the high use of injections could be beliefs and attitudes of patients and health professionals about the efficacy of injection versus oral medication to produce faster onset of action. However, injections are very expensive compared to other dosage forms and require trained personnel for administration. Unhygienic use of injections can increase the risk of transmission of potentially serious pathogens, such as hepatitis, HIV/AIDS, and blood-borne diseases.
“Essential medicines” – A concept adopted by the WHO in 1977 was defined as “those that satisfy the priority healthcare needs of the population.” They are selected with due regard to public health relevance, evidence on efficacy and safety, and comparative cost-effectiveness.”[9] India produced its National Essential Drugs list (EDL) in 1996 and has revised it in 2011 with the title “National List of Essential Medicines” (NLEM). This included 348 medicines which are considered to be adequate to meet the priority health care needs of the general population of the country. The last revision was done in 2015.[8] In the present study, prescribing of drugs from NLEM is lower (75.37%) compared to the one recommended by the WHO (100%), which was parallel with other studies.[17,18,20,21] Nonavailability of the drugs in EML or unavailability of a copy of EML in respective OPDs may be the reason for prescribing other alternatives and use of brand names. Similarly, in the present study, 3.67% prescriptions were found to have recently banned FDCs mentioned in it.[9] The educational intervention of the doctors with standard treatment guidelines is the need of the hour. To address this issue, the government authorities must take necessary steps to ensure proper supply of drugs necessary for the hospital.
The WHO manual[22] has not included diagnosis in core prescription parameters, but it is important to mention diagnosis on a prescription as it reduces confusion. In the present study in (39.67%) prescriptions diagnosis was not mentioned. Like-wise DDF of prescribed medicines is the important parameters. Underdosing will not show any therapeutic effect and excess dose will lead to toxicity. Same is with the frequency and duration. In the present study proper, DDF was not written in 81% of prescriptions. According to the WHO manual, it is the legal duty of the doctor to write legibly.[22] In our set up, all prescriptions were handwritten as there is no facility of computers and 99% prescriptions were legible which is the strong positive finding. Legible handwriting on prescription reduces confusion, lessons the errors by pharmacists regarding dispensing.
The present study could not include prescriptions from emergency department and indoor patient’s prescriptions.
In the present study, most of the prescriptions were found to have generic names. Prescribing practices for antibiotic and injectable drugs show deviation from the standard recommended by the WHO. Minimizing the use of injectables and confining to the NLEM are necessary to further improve the rational use of drugs. Although the handwriting was legible in prescriptions, correct diagnosis, proper DDF was not mentioned in most of the prescriptions. A similar scenario seems to prevail elsewhere in India, and for addressing these issues, the prescribers should be given continued medical education regarding rational use of medicines provide standard treatment guidelines for taking care of these drawbacks. Every hospital should have a working drug and therapeutic committee. Stressing the importance of rational pharmacotherapy in medical curriculum is must to inculcate good prescribing habits in budding doctors.
Subscribe now for latest articles and news.