

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2017.v03i01.003
Year: 2017, Volume: 3, Issue: 1, Pages: 12-18
Original Article
Madhusmita Jena1, Sneha Burela2
Background: A pre-operative diagnosis of the nature of ovarian tumors is not always reliable. Frozen section is a valuable diagnostic tool in rapid intraoperative categorization of ovarian masses and thereby helps in planning the surgical management.
Objective: To categorize ovarian neoplasms into benign, borderline and malignant on frozen sections. To determine the accuracy of the frozen diagnosis by comparing with that of the paraffin hematoxylin and eosin stained sections.
Materials and Methods: Frozen sections on 49 clinically and radiologically diagnosed as ovarian tumors were compared with final histopathogic diagnosis over a period from September 2013 to July 2016 in the Department of Pathology.
Results: Frozen section diagnosis of 49 ovarian specimens, showed 31 (63.2%) benign tumors, 11 (22.4%) borderline tumors and 7 (14.2%) as malignant tumors. The final histopathologic diagnosis revealed 29 (59%) as benign tumors, 08 (16.3%) as borderline tumors and 11 (24.4%) as malignant tumors. The sensitivity and specificity for benign, borderline and malignant tumors on frozen section were 93.5%, 72.7%, 58.3% and 90%, 100%, 100%, respectively. The positive and the negative predictive value for benign, borderline and malignant tumors were 100%, 100%, 100% and 90%, 92.6%, 88%, respectively. The overall accuracy was (44/49) 89.7%. There were no false-positive cases but 5 cases were false negative on frozen. All the 5 discordant cases were mucinous ovarian neoplasms with mean diameter of 26 cm.
Conclusion: With an overall accuracy of 89.7% frozen section is valuable for intraoperative diagnosis of ovarian tumors but has limitations in large mucinous tumors.
KEY WORDS:Accuracy in frozen section, frozen section in ovarian neoplasms, Intraoperative frozen section of ovarian masses
Ovarian cancer has often been called the “silent killer” because of nonspecific symptoms and a lack of trustworthy screening for the early detection. Most of the cases are diagnosed in the advanced stages and require aggressive surgical management.[1]
In ovarian neoplasms such as early stages of epithelial cancer, borderline tumors, and germ cell tumors a conservative approach may be followed particularly in women of reproductive age group whereas in cases of malignant ovarian neoplasms a radical surgery is undertaken. Therefore, an intraoperative diagnosis is crucial in planning for the appropriate surgical management.
Ovarian masses are not amenable to pre-operative biopsy and their cytological sampling is limited to fluid examination if effusion is present. Moreover, a pre-operative evaluation with history taking, physical examination, various imaging studies, and tumor markers or an intraoperative diagnosis by a number of cytological techniques such as imprint, scrape cytology, and intraoperative fine-needle aspiration cytology are less accurate than a frozen section.[2-4]
Although the histopathological diagnosis remains the gold standard technique, an intraoperative diagnosis by frozen section becomes a valuable tool that provides a primary diagnosis of tumors as benign, borderline and malignant and thus guides the operating surgeon in a direction toward the extent of the surgery and also determines the need for a further workup.[3,4]
According to many studies in the literature the overall accuracy of intraoperative frozen section diagnosis for ovarian tumors ranges between 73% and 98%.[3] This study was undertaken to determine the sensitivity, specificity, positive predictive value, negative predictive value and the overall accuracy rate of frozen sections in benign, borderline and malignant ovarian neoplasms at our institute.
After obtaining an approval by the research ethics committee, this study was conducted from the period of September 2013 till July 2016 in the department of pathology where frozen sections were performed on the freshly received specimens of ovarian neoplasms. All the cases which were diagnosed clinically and radiologically as having ovarian tumors and the cases appearing clinically benign with raised CA-125 or alpha-fetoprotein have been included in this study.
The pre-operative data such as clinical history, age, menopausal status, parity, clinical diagnosis, imaging studies, radiological diagnosis, and serum tumor markers, i.e.,CA-125 levels were obtained from the case records. Unfixed or fresh oophorectomy specimens or hysterectomy with salpingo-oophorectomy specimens which were received in the histopathology laboratory were taken for frozen section procedure. Gross morphology of the specimens were observed and recorded.
Representative bits from the ovarian tumor were given which included bits from cystic areas, i.e., cyst wall and bits from solid areas as well. For tumors < 10 cm in size, two bits were given which included the cyst wall and solid areas if present, whereas for tumors greater than 10 cm in greatest dimension four bits, i.e., two bits from the cyst wall and two bits from solid areas were given. The bits taken from the cyst wall were put on the specimen chuck in a swiss roll pattern and were frozen to minus 27°C. Sections of 5-7 μ in thickness were cut as per protocol and stained with hematoxylin and eosin (H&E) stain as well as toluidine blue stain. A frozen section report was given with a specific histologic diagnosis. The specimens were then fixed in formalin. Paraffin blocks of the sections from the specimen as well as of the frozen bits were processed in the routine method and stained with H&E.[5-7] The
final histologic diagnosis of ovarian lesions was based on the WHO classification.[7,8]
The frozen section diagnoses were compared with the final histopathologic diagnoses in each case considering it as gold standard terms.
Concordant cases were those where the diagnosis on frozen sections matched with the final histopathologic diagnosis with regard to the major tumor category (benign, borderline or malignant) for surface epithelial neoplasms and in the case of malignant neoplasms to tumor origin(primary versus metastatic) or to cases in which major histologic category of primary ovarian malignancy such as (germ cell tumor, sex cord stromal tumor) or to benign nonneoplastic conditions(endometriotic cysts).
The discordant cases were those in which incorrect or equivocal assessment could have adversely affected the intraoperative management. These included the false-positive cases (malignant or borderline frozen result, but benign on paraffin sections) and false- negative cases (benign on frozen, but malignant or borderline on paraffin section). Furthermore, those cases which were not recognized as major histologic category of primary ovarian malignancy were considered as discordant.
Statistical analysis Diagnostic parameters such as sensitivity, specificity, positive predictive value, and negative predictive value of frozen section for various categories (benign, borderline, and malignant) neoplasm were calculated using the standard 2 × 2 method. The overall accuracy was defined as the total number of agreements between the frozen section with the final histopathologic diagnosis out of the total number of cases. The cases with discordant diagnosis were reviewed in detail.
Frozen section was performed on a total of 51 cases diagnosed as ovarian neoplasm in the age group ranging from 15 to 80 years with a mean age of 47.5 years. Out of the 51 cases, 2 cases were excluded as they turned out to be tubal masses. As per the clinical data, 22/49 (44.8%) were postmenopausal and 27/49 (55.1%) women. The incidence of parity as per the study was 5/49 (10.2%) were nullipara, 4/49(8.1%) were unmarried females. 10/49cases (20.4%) showed bilaterality. The size of the tumors ranged from 7 to 40 cm across.
On cut section of the tumors, 8 cases (16.6%) showed solid cum cystic areas which included the borderline mucinous tumor, granulosa cell tumor, Sertoli- Leydig cell tumor with heterologous component and mature teratoma, whereas 3 cases (6%) were mainly solid which included the Krukenberg tumor, fibroma, and choriocarcinoma.
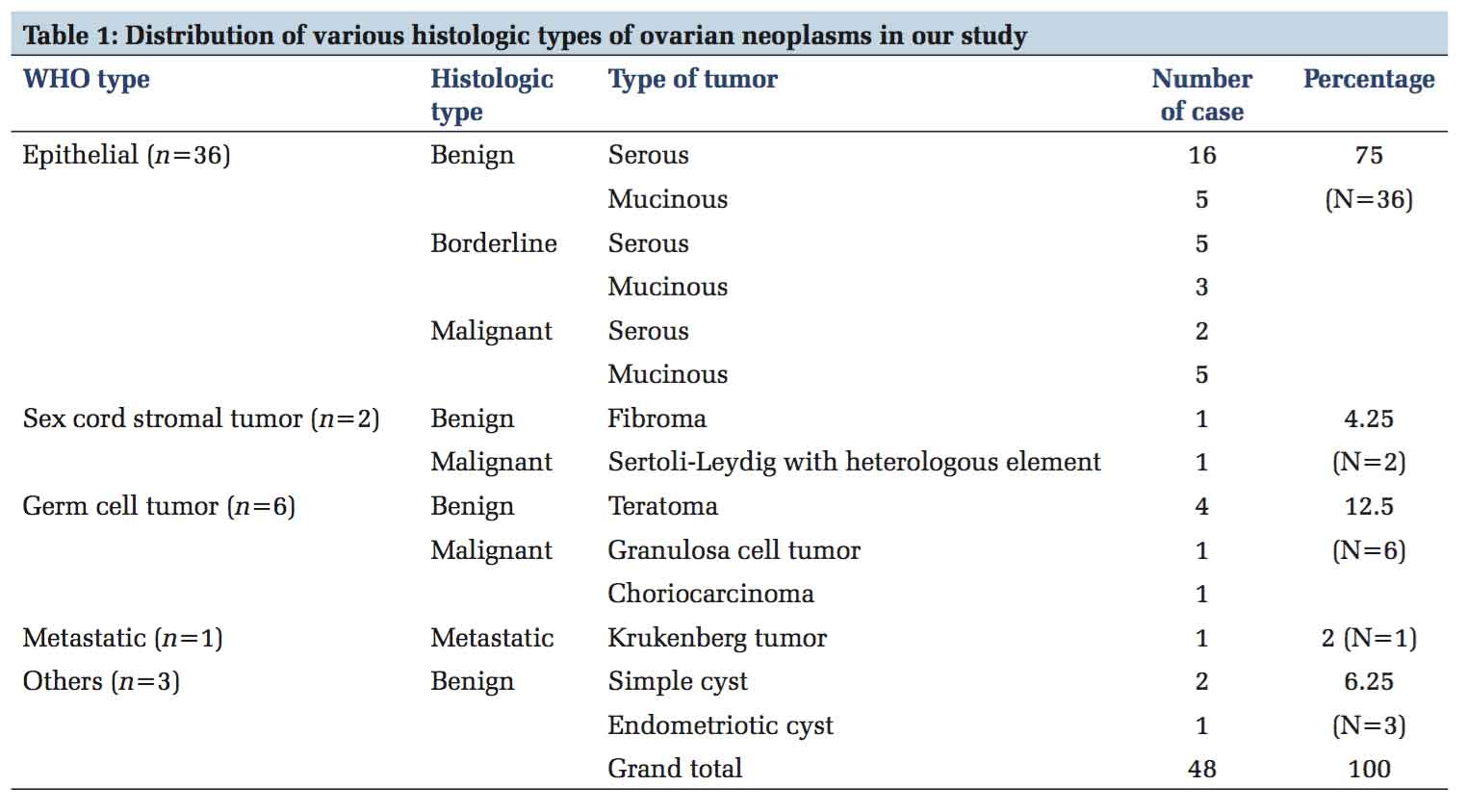
Table1 shows the distribution of the various histologic types of ovarian neoplasms encountered in this study based on the WHO Classification. The epithelial tumors constituted 37/49 (75%) followed by germ cell tumors 6/49(12.5%) of the total ovarian neoplasms. Among the epithelial tumor, the serous tumors (benign, borderline, and malignant) constituted the most common among all the others which accounted for 24/49(48.9%) of the total cases in the study. The mucinous tumors including the benign, borderline, and malignant categories constituted about 13/49 (26.5%).
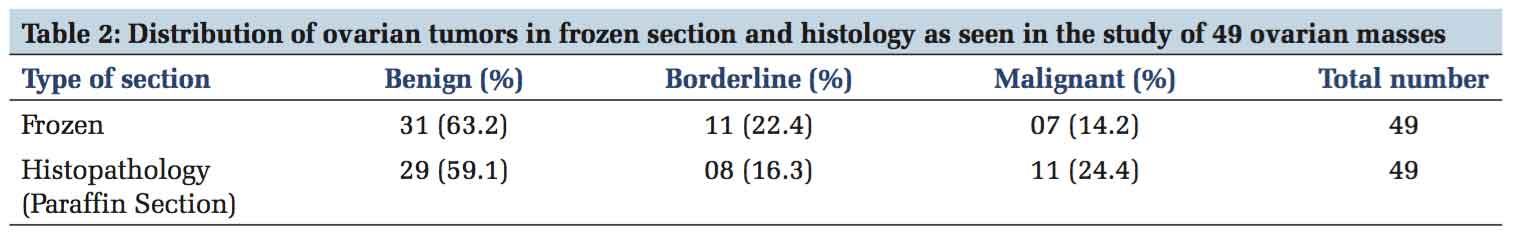
The frozen section diagnosis of 49 ovarian specimens, showed 31(63.2%) benign tumors, 11(22.4%) borderline tumors and 7(14.2%) as malignant tumors. The final histopathologic diagnosis revealed 29 (59%) as benign tumors, 08 (16.3%) as borderline tumors and 12(24.4%) as malignant tumors as shown in Table 2.
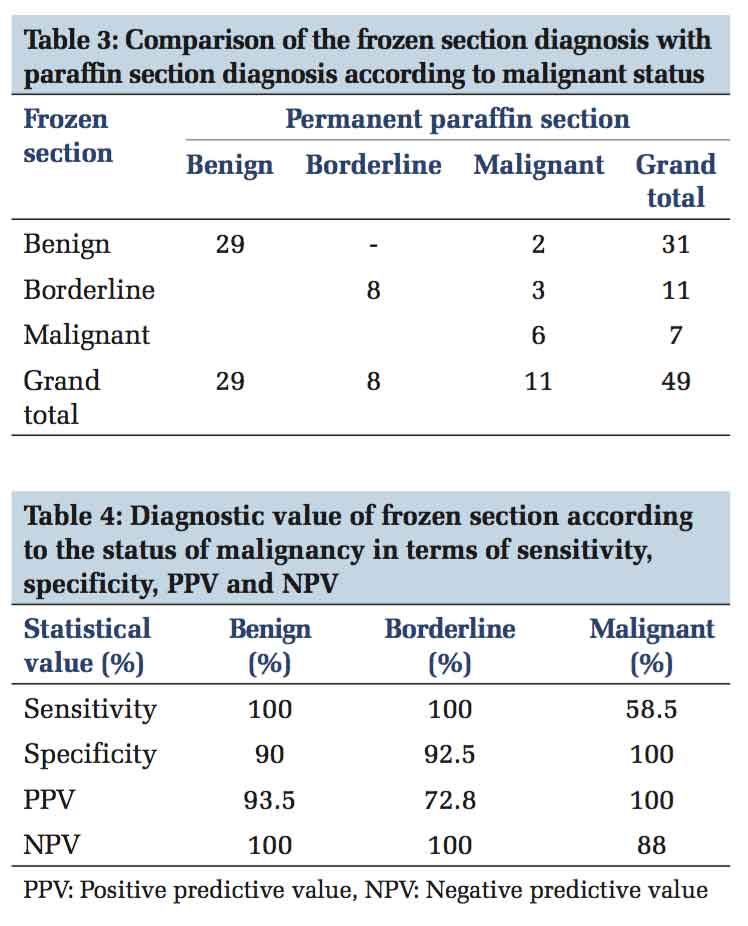
The comparative analysis of frozen section diagnosis with that of permanent paraffin section diagnosis of all the ovarian tumors is shown in Table 3. In this study, 44/49 cases were concordant and 5 cases were discordant between the frozen section diagnosis and the final histopathologic diagnosis. All the five cases were under diagnosed (false negative) by frozen section. Four out of five were mucinous tumors (one benign and three borderline) and the fifth one was a sex cord stromal tumor with a heterologous mucinous component giving a false-negative result of 5/49 (10.2%).
The statistical analysis in terms of sensitivity, specificity, positive predictive value, and negative predictive value of frozen section diagnosis is represented in Table 4.
Table 5 summarizes the statistical details along with accuracy rate of our study compared with that of other studies in the literature.
A correct intraoperative diagnosis of the ovarian masses by frozen section is of great importance and crucial as it can guide the surgeons to avoid under treatment or overtreatment of the patients. This is particularly useful in young women who desire fertility, in borderline tumors and in some cases of endometriosis of ovary which mimics as malignancy.[2,3,7] As pre-operative diagnosis of ovarian masses is not always reliable, this study was carried out on 51 cases of ovarian masses to assess the accuracy of the frozen section at our institute and thereby review over the discordant cases in details and also to look into the factors affecting the accuracy of the frozen section. Two cases were excluded from the study which turned out to be tubal masses on histology.
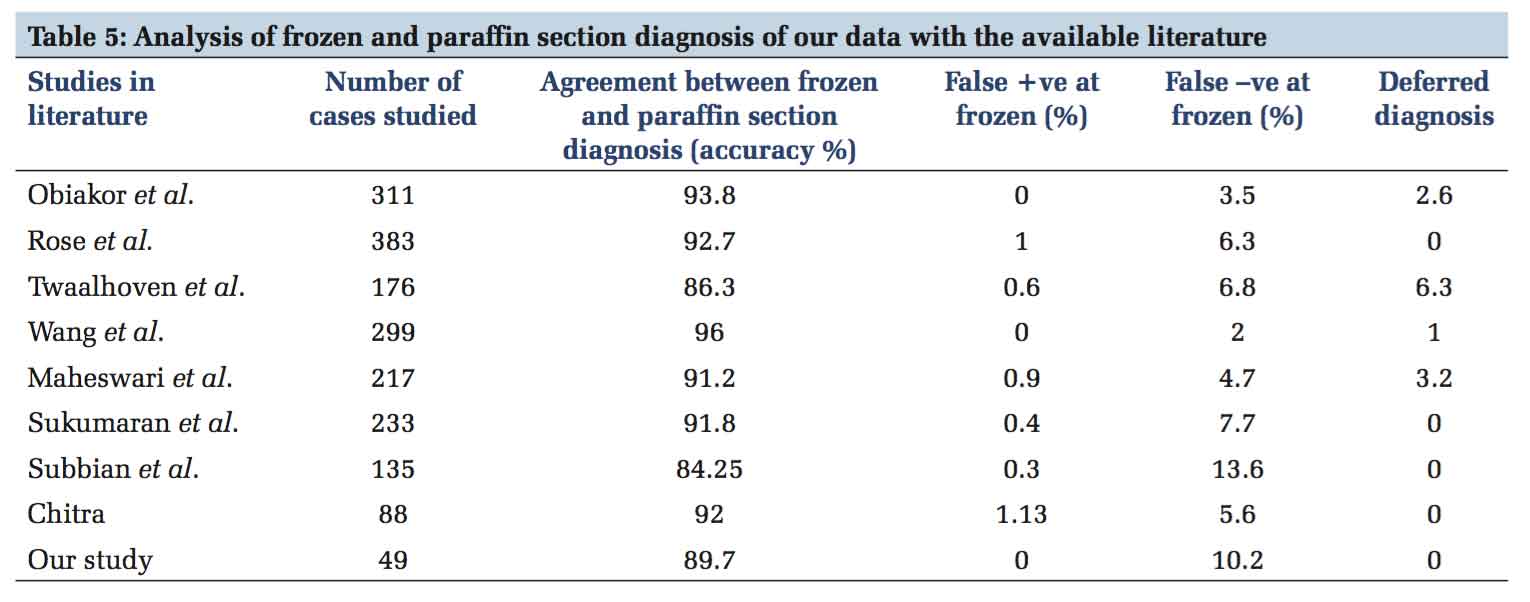
The overall accuracy of the frozen section diagnosis for ovarian tumors reported by most studies range from 73.8% to 98.7%.[2,3,7,9-14] Our study showed an overall accuracy of 89.7% which is within limit of the accuracy range from the literature.
There were no false-positive cases in our study. We observed that out of 5 false-negatives, 4 cases were mucinous tumors, and the other one was a sex cord stromal tumor with heterologous mucinous component giving a false-negative result of 10.2% which was consistent with the false-negative rates of other studies that ranged from 2% to 13.6%.[3,7,10-14]
A published meta-analysis of 18 studies comparing frozen section diagnosis of ovarian pathology with the final histopathology showed the sensitivity of frozen section for benign and malignant lesions to vary from 65% to 97% and 71% to 100%, respectively.[16] Our study showed a sensitivity of 93.5% and 58.3% for benign and malignant lesions of ovary, respectively, on frozen section. The low sensitivity for malignant lesions was due to high rate of false negatives as observed in 3 borderline mucinous tumors and one benign mucinous cystadenoma on frozen section which were later categorized as malignant on histology on the basis of microinvasion.
The factors which can affect the frozen section are sampling error, technical error, and interpretation error.[2,9,11] In two of the mucinous borderline tumors of the intestinal type, the stromal microinvasion on frozen section could not be interpreted because even at paraffin section histology, the out pouching of the epithelium and formation of secondary glands make the assessment of stromal invasion in mucinous tumors more difficult than in the serous tumors.[17]
Given the difficulty in distinguishing borderline from invasive malignant tumors, the use of the term” at least borderline” as a reasonable frozen section opinion indicates that the final diagnosis may change but allows the surgeon to proceed with a staging operation which averts a second surgery.[9]
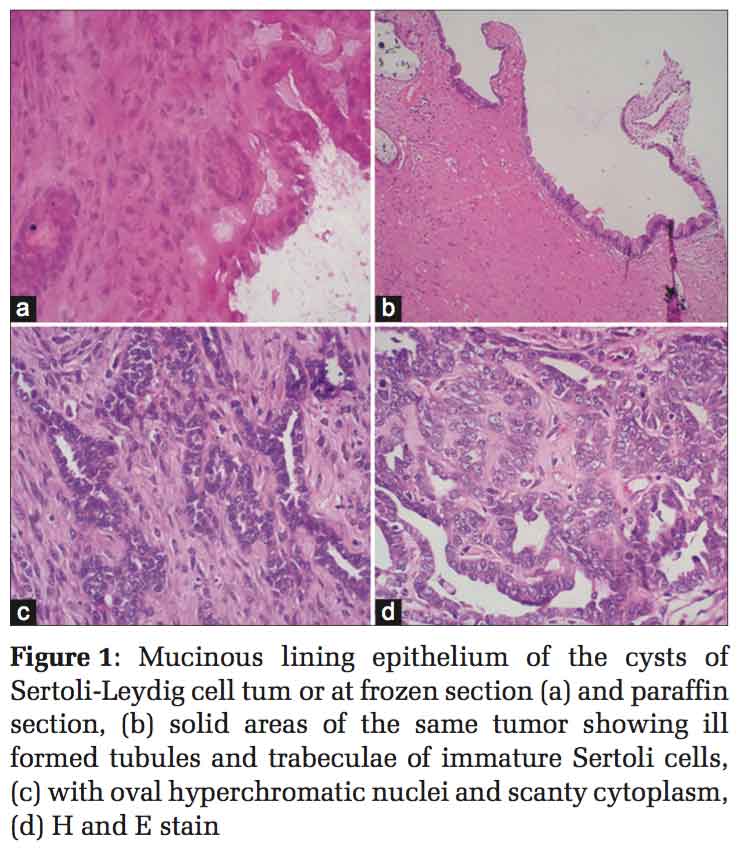
Error in interpretation was identified in two cases reported as benign on frozen, one of which was in Sertoli-Leydig with heterologous element where a mucinous element was interpreted as benign mucinous cystadenoma as shown in Figure 1. The other one was a mucinous tumor (benign at frozen section) which showed focus of microinvasion on paraffin histology and reported as malignant.
Thus, two patients out of the 49 patients called benign by frozen section, the diagnosis was changed to malignant with an implication that these patients were probably undertreated at the initial surgery. One of them became a low-grade mucinous tumor on histology where surgical treatment would have remained the same as performed for the benign diagnosis on the frozen section because the woman was postmenopausal. As per literature, a high proportion of mucinous tumors can show a variety of patterns such as an admixture of benign and borderline areas, borderline with foci of frankly invasive carcinoma and sometimes a complete range of appearances containing benign epithelium, areas of borderline malignancy and focal invasive carcinoma.[17] The other case of sex cord stromal tumor with heterologous element which became malignant on histology was mainly an interpretation error because on the gross morphology the ovarian mass was very large (25 cm × 15 cm) multiloculated with mucinous fluid and showed benign mucinous element on frozen section. The areas of Sertoli- Leydig cell element surrounding the mucinous component was interpreted as stromal element on frozen section possibly due to the thickness, foldings of the section, and lack of expertise on frozen section diagnosis.
As in some other studies, this study too showed that all the disagreement between frozen section diagnosis and final paraffin diagnosis were in large mucinous tumors where the mean diameter was around 25 cm.[2,12] Under-diagnosis in case of borderline ovarian tumors usually occurs as a result of under-sampling. As WHO criteria for the diagnosis of borderline mucinous tumors is quantitative (>10 % of tumors examined showing atypical proliferative features in the absence of frank invasion), it can be misinterpreted in limited sections available on the frozen section.[15] The sampling error can be minimized by performing multiple sections of at least one section for every 10 cm size of the mass.[13,15] However, multiple frozen section may not be able to eliminate the discordant cases as seen in our study where multiple sections up to 4 were taken. Furthermore, performing many frozen sections in each case is not practical as it is time consuming. As seen in this study, in a case of solid ovarian mass of choriocarcinoma, even multiple bits on frozen section showed mainly areas of necrosis with occasional clusters of malignant cells and categorization of these cases becomes difficult. Hence, in large tumors, in spite of many bits taken for frozen section, there is a possibility of discordance.
The incidence of over-diagnosis is rare with some examples showing tangential cutting leading to false impression of invasion.[15]
In our study, none of the cases with overt/frank malignancy on histology (paraffin section) were missed at frozen section or in other words the accuracy of malignant tumor on frozen section diagnosis was high, with no benign or borderline tumors being misdiagnosed as malignancy.
The sensitivity of borderline tumors in most studies have been found to be low in the range from 44.4% to 77.2%, but a considerable improvement has been noted in the recent years.[3] In our study, the sensitivity for the borderline tumors was 72.7% due to three cases becoming malignant on histology. The reason for false-negative results on borderline tumors has been explained in the previous paragraphs.
Published literature indicates that gynecologic frozen section diagnosis is sufficiently sensitive and specific with agreement rates ranging from 86.3% to 96%, with low false-negative rates and more reassuringly even low false-positive rates (0-1%) as shown in Table 5.[2,3,4,7,11-14]
This study of frozen section on ovarian masses with a diagnostic accuracy of 89.7% is definitely an eye opener for the gynecologic surgeons regarding the usefulness of this diagnostic tool. Furthermore, it highlights that intraoperative reporting of histology on cryostat sections, the pathologist contributes in helping the surgeons for tailoring the surgery. Although the study was done on a small sample size, but it shows that frozen section can be an effective diagnostic tool if utilized judiciously by the pathologists and surgeons by knowing its advantages and limitations.
The authors would like to thank Mr. Harish, Senior Laboratory Tehnician and the Staff of the Department of Obstetrics and Gynecology, MVJ Medical College and Research Hospital, Bengaluru, Karnataka, India.
Subscribe now for latest articles and news.