Introduction
Use of aircraft for medical evacuation has increased in last two decades 1. International Civil Aviation organization defines aeromedical transportation (AMT) as the movement of patients, organs, blood, tissue, medical supplies, or medical personnel by aero plane or helicopter 2. It can be further classified into air ambulance (AA) and helicopter emergency medical services (HEMS). The urgency of the requirement, distance of the landing facility determines the type of Aeromedical transport. The usage of this mode by the defense establishments is quiet common as compared to civilian setup. So the challenges experienced by the health care providers during air transfer may be a valuable insight to the upcoming usage of this mode in the civilian sector as well. The objective of this study is to provide an experience of aeromedical transportation of 100 critically ill cases over a period of a 5 years and its associated challenges, troubleshooting measures that provide an insight into this domain and also to discuss various practical aspect of safe transfer of patient to definitive health care center.
Methods
After obtaining ethical committee’s approval, hospital records of all air medical transportation undertaken to the institute during the period were analyzed for demographics, primary etiology, and events during transport. Predetermined demographic and variable parameters were accessed from medical records of the hospital after due clearance from hospital authorities and fed into an Excel sheet for analysis.
All intubated Critical patients requiring definitive and super specialty medical care, transferred by air during Jan 2016 to Dec year 2020, analyzed in this retrospective study. All these intubated patients were transferred after a decision of trauma team from mountainous high altitude area to tertiary care hospital by fixed wing air- craft or by helicopter (and critical care specialist along with assistants). All patients were ventilated en route by Bains circuit and kept sedated. Patient were monitored with recording of their pulse rate and saturation. Few patients received inotropic support by infusion pumps for maintaining their blood pressure en route. Trauma team was trained and was having skill for mechanical ventilation, advance cardiac life support, advance trauma life support, for blood transfusion in route and continuation of inotropic infusion. Team members were specifically trained for CPR. All patient were given sedation in form of injection fentanyl 1mcg/kg in dividing doses and boluses of propofol 10 mg intravenously during transfer.
Results
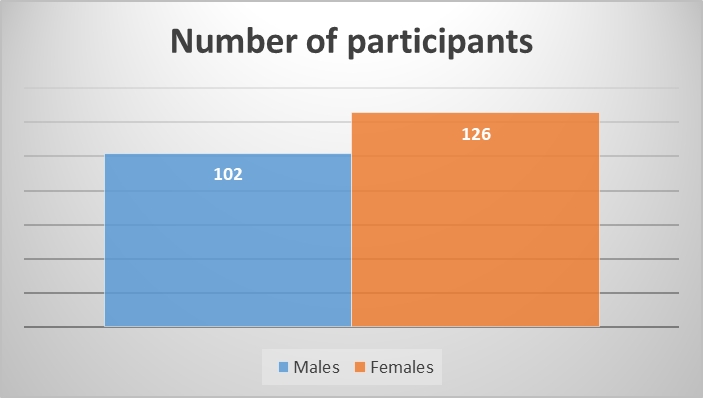
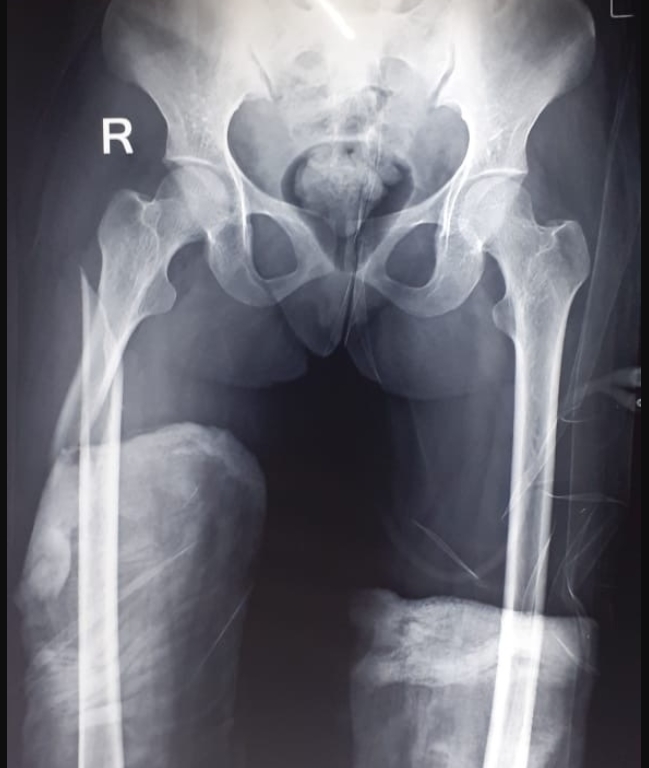
A total of 100 patients were transferred by us to tertiary level hospital. Mean age of males was 36.7 ± 11.6 yrs and mean age of females was 22.4 ± 5.8 yrs. Patient profile comprised of 96 percent males and 4 percent females. Majority of transfer was for head injury 35%, Polytrauma 27% gunshot wound chest/ abdomen 17 % Other were cases of patient requiring support of nephrologist, burn, reconstructive unit. One patient was a case of long bone injury with clinical evidence of fat embolism syndrome (Table 1).
|
Variable |
Value (%) |
|
Total patients |
100 |
|
Mean age of males in years (mean ± SD) |
36.7 ± 11.6 |
|
Mean age of females in years (mean ± SD) |
22.4 ± 5.8 |
|
Male:female |
96(96%):4(4%) |
|
Total flying time (min) |
8310 |
|
Avg evacuation time (min) |
83 ± 7.6 |
|
Helicopter/ Fixed Wing Aircraft |
76(76%)/24(24%) |
All patient transferred had hemoglobin more than 9 gm/dl. Oxygen saturation dropped and remained between 74- 88 % along with rise or fall of heart beat (up to 20 % of the basal) while flying above 10000 feet. All patients were having endotracheal tube and were ventilated by Bain’s circuit keeping oxygen flow to 5-15 litre/min with ventilation rate of 12 -22 / min. We felt the need of increasing oxygen flow to 8-15 liter/min and ventilation rate to 14-22 to maintain higher Spo2 concentration. The Spo2 increased gradually with lowering altitude of helicopter requiring less oxygen flow and ventilation. The total duration of flight was between 40 – 150 min and average being 83 min. Twenty four patients were transferred by fixed wing aircraft and rest 76 by helicopters (Table 2)
|
Etiology |
Number (%) |
|
Cardiovascular disease |
06(6) |
|
Central nervous disease |
05(5) |
|
Multiorgan medical disease |
09(9) |
|
Polytrauma without head Injury |
27(27) |
|
Isolated head injury |
33(33) |
|
Gunshot wound chest/abdomen |
14(15) |
|
Others |
06(6) |
The most common change noticed was fall in oxygen saturation with incidence almost 100% of the patients. The mean fall in saturation was 17.29%. Four patients required injection atropine for bradycardia which resulted from decrease of SpO2. The flying time above 10000 feet was for 12–15 min only in entire travel time by helicopter and desaturation and change of heart rate was seen during this period mostly. The measurement of axillary temperature was done and mild hypothermic fall was experienced in all the patients transferred by helicopter mean 96.6 (Range-95.6-98 degree F). The problems of noise induced discomfort (74% reported), difficulty in communication (80% reported) due to ambient noise and discomfort due to cold temperature (90.5% reported) was reported by the health care providers. As per patient related factor the most problematic experience was the difficulty in obtaining continuous SpO2 readings as reported by the health care providers. The service satisfaction was more in fixed wing aircraft as compared to HEMS. All except two patients transferred by us both by fixed wing aircraft or helicopter from remote Himalayan mountainous region to definitive care hospital could reach tertiary care hospital without complication on board or any morbidity. One patient with a diagnosis of long bone fracture with fat embolism syndrome developed cardiac arrest just before landing and was resuscitated successfully but developed some amount of permanent hypoxic damage to brain. One patient with tracheostomy also had sudden cardiac arrest at receiving center and the cause was removal of tracheostomy tube from trachea due to pull while unloading from ambulance. The patient was given CPR and revived successfully. So we experienced a complication rate of 6.3% in our experience of transferring patient by air
Discussion
The need for the medical transportation of the patients through air has increase in the last twenty years. 3 The use of air transport to provide medical evacuation on the battlefield dates to First World War and continued during the Korean and Vietnam wars. 4 Later on, aircraft began to be used for the civilian emergency medical services. Aeromedical evacuation (AE) is referred to the long-distance usually greater than 300 miles, air transportation of patients after medical treatment that is adequate to assure a successful movement. AE is inherently different than medical evacuation (MEDEVAC), which refers to the emergency transportation of patients to the nearest appropriately equipped medical facility prior to definitive treatment. 2 Our complication rate (6.3%) is comparable to other studies. 5 Szem et al. reported a complication rate of 5- 6%. 6 This paper however evaluated interhospital road transport of patients. A review article by Waydhas reported a complication rate in the range of 6-70% during transfers rather than during actual transport. 7 Most common complications were disconnections of leads, intravenous tubing, and ventilator circuits. We can safely say that air transportation carries no more risk than ground transportation.
In India air medical transportation facilitated massive evacuation exercise undertaken by the Indian forces in Uttarakhand and Kashmir in recent times. Many more patients are transported daily in need of advanced medical attention to higher centers worldwide. These are inter-hospital transfers of critical patients using the available air infrastructure. Air evacuation team provide comprehensive pre hospital and emergency and critical care to all types of patients during aeromedical evacuation or rescue operations aboard helicopter and propeller aircraft or jet aircraft.
Many patients are transferred from remote field location to definitive health care facilities belong to poly-trauma cases due to road traffic accidents, gunshot wounds, mine blast injuries, grenade injuries, burn cases and few medical disease cases. There is paucity of investigation services like MRI, CT SCAN and few specialized sets of investigations which necessitate transfer of the critically ill. There are other instances of transferring for definitive care by neurosurgeon, reconstructive, maxillofacial, gastrointestinal surgeons, as they are often not available in peripher al locations. 3
Type of transfer
Transport of patient by fixed wing aircraft for long distances is possible when there is facility of a nearby airport is in existence. This mode of transfer is safe as the fixed wing aircraft is pressurized (Cabin pressurization: conditioned air is pushed inside the cabin of an aircraft to maintain normal atmospheric pressure, temperature and humidity to create a safe and comfortable environment for passengers) and have greater space for patient positioning and less vibration. 8 As the aircraft is pressurized there is negligible chance of effect of altitude and atmospheric pressure over critical patient. Often these air ambulances are specially designed, and they carry patient transport unit (PTU) with facility of special wheeled trolley having multipara monitor, infusion pumps, and oxygen cylinders with oxygen delivery system, suction apparatus and defibrillator. 4 Vital signs can be recorded at constant intervals by multipara monitor and all medical support is possible due to availability of all essential equipment and drugs on board.
Transport by helicopter is other alternative employed for shorter distances in field areas and remote locality for transfer of critically ill from primary location to nearby hospital or to a definitive health care facility having all specialties. Transfer by helicopter is transport of a critical patient and this is an example of transfer in non-pressurized where cabin pressure, temperature and humidity cannot be maintained and follows the effect of altitude for the parameters mentioned. There are many physiological hazards due to altitude effect like hypoxia, hyperventilation, decompression sickness, spatial disorientation, hypothermia, effect of noise and vibration. 3 Presence of higher ranges of Himalayas often necessitates flying at more than 10000 feet in these remote mountainous areas.
Effect of altitude leading to hypoxia
Normal atmospheric pressure at sea level is 760mm of Hg/14.7 PSI. With height atmosphere becomes less dense and pressure falls. At 10000 feet atmospheric pressure is 523 mm of Hg/ 10.10 PSI and at 12000 feet 483.4/9. 34 PSI. A normal individual can show and adjust due to physiological reserve up to 12500 feet of altitude and can show minor problems like trapped gases (ears, sinus, and GI tract). 9 There is feeling of shortness of breath, headache, fatigue and dizziness at this height which is felt by trauma team transferring the critically ill. Effect is profound over critically ill due to loss of physiological reserve and damage to vital organs. 10
Hypothermia
There is chance of hypothermia as the change of atmospheric pressure is around 2 degree centigrade/ 1000 feet of height as compared to the corresponding ground temperature. 11 Thus if the ground temp at Himalayan region is 15-20 degree then the corresponding temp at 10000 feet will be -5 to 0 degree. Thus, chance of lowering of temperature is more in case of snow, cloud or rain. Precaution in form of layers of warm blanket is required to be put over the scoop stretcher carrying patient. Warm fluids should be administered in route also. There is no facility to run patient warmer inside a helicopter and space is scarce. Pre heated electric blanket or special mattress which remains warm can be applied to patient to prevent hypothermia.
Transfer of patient from hospital to helicopter
Before transferring, emergency bag should be checked for airways supraglottic and infraglottic, essential drugs (for sedation, inotropic support), drugs required in emergency for resuscitation, laryngoscope, dry batteries, fixing tapes, fluid bottle and resuscitation bag. Oxygen cylinder gauge pressure along with Bain’s circuits should be checked. Ideally full oxygen cylinder should be attached and additional cylinders should be loaded in ambulance with their changing wrenches to be carried in the helicopter. It is practical to use bull nose fitting without humidifier. There will be less chance of water going into the inner tube of Bain’s circuit, at the time of transferring as a result of gravity. All essential drugs for sedation and for resuscitation should be kept loaded in syringes in appropriate dilution in a tray for ready use if required inside the helicopter. A relatively experienced and skilled assistant at least 2 years of training in critical care, should accompany anesthesiologist inside the helicopter. Finger held Spo2 and heart rate monitor along with multi Para- monitor should be attached to the patient for monitoring of vital parameters. Oscillometric type of blood pressure recording is not effective inside the helicopter as a result of vibration of rotors. 12 Pulse palpation and heat rate auscultation is equally difficult due to noise and vibration. S shaped wire hooks should be available for hanging fluid bottles with the roof channel of helicopter as is contains holes into it.
Fluid administration, care of body tubes and lines
Warm fluids should be used and there rate of infusion should be checked as the rate of drops/ min varies as per the altitude of flying helicopter due to change of atmospheric pressure. Inotropic support present should be ideally continued by infusion pumps having good battery backup and automatic flow not dependent on gravitational flow. Chest tube should be clamped at the time of loading and unloading the patient from ICU to Ambulance and from ambulance to helicopter vice versa. Urinary bag should be emptied and urine output should be entered in the case sheet. Arterial line should be closed, rolled and secured nicely using bandages if present. All wound drains should be secured.
Care of airway
Endotracheal airway is ideal and practically more suitable. They should be secured nicely and special care should be taken so that they may not get any pull or pressure during transport. Similarly, if tracheostomy tube is present, it should be secured nicely and catheter mount can be attached to it and should be secured nicely over the chest of patient with a band. Special care should be taken to prevent any pull over tracheostomy tube during transport as it can come out of trachea and can go into false passage. Before transfer airway should be suctioned as a routine protocol. Laryngoscope and other airway should be handy in case of accidental extubation. Cuff pressure should be checked and there is chance of expansion in higher altitude.
Patient positioning
In all patient of polytrauma hard collar should be applied over neck and protection for spine should be taken, care of lower limb fracture application of Thomas splint is equally important. While transferring any person with long bone fracture and diagnosis of fat embolism, airway should be secured as there is chance of further spillage of fat globules into circulation due to vibration inside the helicopter. 4 Cap should be applied over head with a cushion of cotton to prevent effect of cold and prevention against injury. Eyes should be covered too to prevent introduction of any foreign particles and exposure keratitis.
Administrative coordination
Constant communication between trauma transfer team and administration controlling arrival of helicopter at helipad/ fixed wing aircraft at airport and landing at definitive health care facility is needed. There should be synchronization in all aspect; a standing ambulance with a critically ill waiting at helipad can be hazardous. Once a helicopter or fixed wing aircraft takes off for a certain definitive health care facility, the same should be communicated to administrative staff of health care. A collection trauma team with ambulance and equipment should be ready at airport/ helipad near the transferred health care facility for prompt transfer to the ICU of hospital. Director General Of Civil Aviation Guidelines (DGCA 2015) 13 gives details of equipment and manpower required for aeromedical evacuation.
Conclusion
Knowledge of changes at different altitude and their physiological effect over a critically ill patient will guide trauma transfer team to take appropriate steps to prevent any morbidity to the patient and a problem free transfer. Air medical transport carries no more risk than ground transportation.14 Our aim to transfer them to definitive health care could be achieved by following standard operating procedures developed by trauma transport team. Evacuation by helicopter is very fast and it can reach to remote place for evacuation of a critically ill patient. Helicopter evacuation can reduce mortality, morbidity as well as reduce chance of disabilities too.