Introduction
Paranasal sinuses (PNS) are the air-filled cavities around the nasal cavity within the facial bone and within the skull. These are maxillary sinus (largest), ethmoid sinus, frontal sinus and sphenoid sinus. There are few imaging modalities for the assessment of these sinuses. Previously, conventional radiography of the skull with various projections was used before the advent of Computed Tomography (CT). Due to limited evaluation of the ethmoid sinus, sphenoid sinus and osteomeatal complex (OMC) by conventional radiography, CT scan widely gained acceptance.1 Multiplanar high resolution CT (HRCT) has the excellent ability to delineate both bony anatomic details as well as pathology involving the PNS. Precise knowledge of anatomy of the PNS is essential for the radiologist and for the sinus surgeon.2 It provides a preoperative roadmap for the endoscopic sinus surgeon. However, there is always an increased radiation dose to the lens and thyroid gland, so care should be taken to minimize the radiation dose to these organs. Radiation dose by ‘low dose sinus CT protocol’ was found to be 5.53+/-0.82 mGy for lens and 0.63+/-0.43 mGy for thyroid as compared to the ‘standard sinus CT protocol’. 3
There are multiple anatomic variants of paranasal sinuses and commonly visualized in the CT scan of PNS.4, 5 Common variations are deviated nasal septum, agger nasi cells, haller cells, onodi cells and concha bullosa.6 Uncommon variations include pneumatization of the uncinate process, large ethmoid bulla, supra-orbital cells, crista galli and even in the hard palate and nasal septum. 7, 8
Some of the variations have been reported to be associated with chronic rhinosinusitis due to stenosis of the drainage pathway. However, several studies show no significant correlation with rhinosinusitis. 9
Failure to recognize certain variations like onodi cells, haller cells, deep olfactory groove, pneumatised anterior clinoid process etc. will lead to postoperative complications. 6, 10, 11
The purpose of this study is to determine the frequency of anatomic variations of paranasal sinuses and nasal cavity and also to correlate their association with radiological significant sinonasal mucosal disease in our population (Eastern India).
Methods
It was a retrospective & descriptive study. The study has been approved by the Institutional Ethical Committee (IEC). Data was collected from the past one year (January 2019 – December 2019) stored in the PACS (picture archiving and communicating system) in the Radiodiagnosis department and from the medical record section for the clinical history.
The images were reviewed by two experienced radiologists (6-8 years of experience) using multiplanar reconstructions (in axial, sagittal and coronal section) in bone and soft tissue windows. Images were analysed for the following details – deviated nasal septum, agger nasi, pneumatised uncinate process, bulla ethmoidalis, concha bullosa, paradoxical middle turbinate, haller cell, onodi cell, supraorbital cell, pneumatization of the crista galli, clinoid process, pterygoid plate and hard palate etc.
One hundred and twenty five cases of age more than 15 years were included in this study who underwent CT PNS study for clinical history of rhinosinusitis of varying severity from the ENT and General Medicine department. Sinus infections and neoplasm not destructing the bone or/and not altering the PNS anatomy were included in this study.
Patients underwent sinus surgery, facial trauma and malignancy or infection leading to bony destruction of PNS were excluded from the study. Patients of paediatric age groups were also excluded from the study because of ongoing development of the sinuses.
The machine used was a 128-slice helical MDCT (Toshiba Aquallion) scanner. Plain (without contrast) CT as well as plain and contrast-enhanced CT scans both were evaluated.
All the data was entered into the Microsoft excel sheet and the data were analyzed. Analysis toolpak software was used for calculation of p- value, whenever necessary. Association of frequency of anatomic variations and radiological evident mucosal diseases were calculated by using regression analysis.
Frequency of occurrence of all the sinonasal variations was compared between patients who were having minimal or no apparent radiological evidence of rhinosinusitis and those having radiological evidence of moderate to significant rhinosinusitis.
Results
CT images of 125 patients were evaluated in which 78 (62.4%) were male and 47 (37.6%) were female.
|
Age range |
Number of cases |
Percentages (%) |
|
15-24 |
52 |
41.6 |
|
25-34 |
28 |
22.4 |
|
35-44 |
16 |
12.8 |
|
45-54 |
15 |
12 |
|
55-64 |
7 |
5.6 |
|
65-74 |
4 |
3.2 |
|
75-84 |
3 |
2.4 |
Age range was 15-80 years. Mean age was 32.14+-15.99 years. Maximum numbers of cases fall in the age range of 15 – 24 yrs.
|
Param- eters |
No or minimal mucosal disease |
Moderate to significant mucosal diseases |
||
|
Number of pati- ents |
30 |
Male - 16 |
95 |
Male - 62 |
|
Female - 14 |
Female - 33 |
|||
|
|
|
|
|
|
|
Age range |
15-64 years |
20-84 years |
||
|
|
|
|
||
|
Mean age |
31.91±15.99 years |
31.94±15.95 years |
||
No or minimal mucosal disease were found in 24% of patients with age-range 15-64 years and moderate to significant mucosal diseases were found in 76% patients with age-range 20-84 years irrespective of presence or absence of anatomical variants of paranasal sinuses.
|
PNS Variations |
Pre sent |
No or minimal mucosal disease (n=30) |
Moderate to signi ficant mucosal diseases (n=95) |
P - value |
|
Deviated Nasal Septum |
50 |
8 (16 %) |
42 (84 %) |
0.049 |
|
Nasal Septal spur |
61 |
14 (22.95 %) |
47 (77.05 %) |
0.027 |
|
Concha bullosa |
32 |
7 (21.88 %) |
25 (78.12 %) |
0.54 |
|
Paradoxical middle turbinate |
28 |
9 (32.14 %) |
19 (67.86 %) |
0.77 |
|
Agger nasi |
74 |
16 (21.62 %) |
58 (78.38 %) |
0.16 |
|
Haller cells |
9 |
1 (11.11 %) |
8 (88.89 %) |
0.59 |
|
Onodi cells |
19 |
2 (10.53 %) |
17 (89.47 %) |
0.24 |
|
Ethmoid bullosa |
60 |
15 (25 %) |
45 (75 %) |
0.13 |
|
Intersphenoid septal deviation |
28 |
9 (32.14 %) |
19 (67.86 %) |
0.37 |
|
Optic nerve deviation |
12 |
2 (16.67 %) |
10 (83.33 %) |
0.64 |
|
Vidian nerve deviation |
20 |
2 (10 %) |
18 (90 %) |
0.75 |
|
Supra-orbital cells |
52 |
9 (17.31 %) |
43 (82.69 %) |
0.12 |
|
Pneumatiz- ation of |
|
|
|
|
|
1. Anterior clinoid process |
44 |
10 (22.73 %) |
34 (77.27 %) |
0.97 |
|
2. Pterygoid plate |
41 |
12 (29.27 %) |
29 (70.73 %) |
0.44 |
|
3. Crista galli |
6 |
0 (0 %) |
6 (100 %) |
0.89 |
|
4. Dorsum sella |
10 |
3 (30 %) |
7 (70 %) |
0.85 |
|
5. Hard palate |
28 |
5 (17.86 %) |
23 (82.14 %) |
0.63 |
Frequency of occurrences of paranasal sinuses variations were more in patients with moderate to significant mucosal disease. P value for DNS (deviated nasal septum) and nasal septal spur were <0.05, indicating statistically significant correlation.
|
PNS Variations |
Total |
Unilateral (%) |
Bilateral (%) |
|
Concha bullosa |
32 |
21 (65.63 %) |
11 (34.37 %) |
|
Paradoxical middle turbinate |
28 |
14 (50 %) |
14 (50 %) |
|
Agger nasi |
74 |
16 (21.62 %) |
58 (78.38 %) |
|
Haller cells |
9 |
3 (33.34 %) |
6 (66.66 %) |
|
Onodi cells |
19 |
10 (52.63 %) |
9 (47.37 %) |
|
Ethmoid bullosa |
60 |
10 (16.67 %) |
50 (83.33 %) |
|
Optic nerve deviation |
12 |
11 (91.67 %) |
1 (8.33 %) |
|
Vidian nerve deviation |
20 |
10 (50 %) |
10 (50 %) |
|
Supra-orbital cells |
52 |
12 (23.08 %) |
40 (76.92 %) |
|
Pneumatization of |
|
|
|
|
1. Anterior clinoid process |
44 |
14 (31.82 %) |
30 (68.18 %) |
|
2. Pterygoid process |
41 |
20 (48.78 %) |
21 (51.22 %) |
|
3. Hard palate |
28 |
3 (10.71 %) |
25 (89.29 %) |
|
Lamina papyracea dehiscence |
28 |
5 (17.86 %) |
23 (82.14 %) |
Concha bullosa and pneumatisation of pterygoid process were commonly unilateral. Whereas bilateral variation was found to be greater in agger nasi followed by ethmoid bullosa.
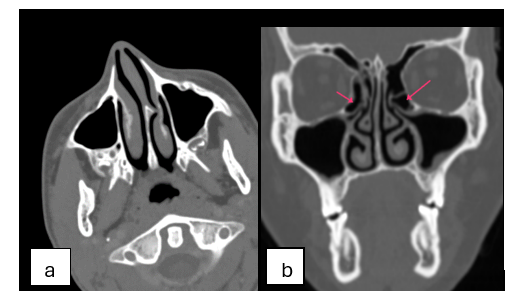
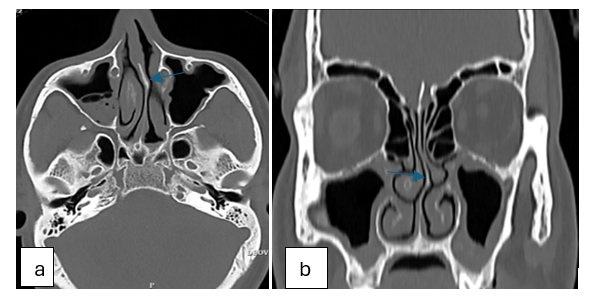
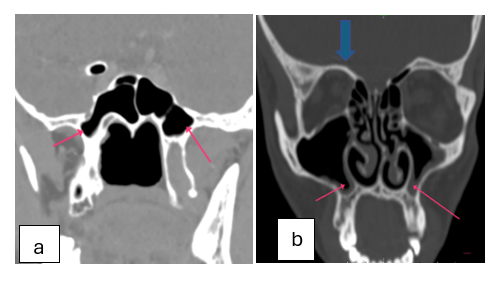
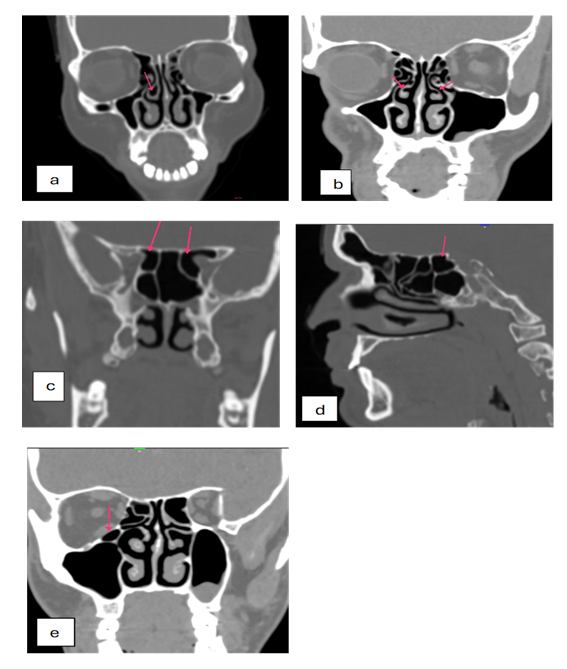
The most common anatomic variations were agger nasi, nasal septal spur (Figure 1 a), ethmoid bullosa (Figure 1 b), supra-orbital cells, deviated nasal septum (Figure 2 a & b) and pneumatization of anterior clinod process (35.2%), pterygoid process (32.8%) (Figure 3 a) and hard palate (22.4 %) (Figure 3 b) in their decreasing frequency. The least common variations were concha bullosa (25.6%) (Figure 4 a), paradoxical middle turbinate (22.4 %) (Figure 4 b), Intersphenoid septal deviation (22.4 %), optic nerve (9.6%) (Figure 4 c) and vidian nerve (16%) deviation, onodi cells (15.2%) (Figure 4 d), haller cells (7.2%) (Figure 4 e), pneumatization of dorsa sella (8%) and crista galli (4.8%) & dehiscence of lamina papyracea (22.4 %). In some cases, we also found the presence of hypoplasia of maxillary sinus (2 cases), frontal sinus (4 cases) and sphenoid sinus (1 case), absent frontal sinuses in 6 cases & sinus septation (maxillary, frontal and ethmoid) in 28 cases. Sphenoid sinus septation was seen in 12 patients.
Discussion
The most common anatomic variation was agger nasi cells in our study which constituted 59.2% (74 out of 125) of the study population. Among them 78.38% were bilateral and 21.62% were unilateral (56.25% on the left side among these). Minimal or no sinusitis was seen in 16 (21.62%) and moderate to significant sinusitis was present in 58 (78.38%) patients with insignificant p value (0.16). Hence no significant correlation was found between the sinusitis and agger nasi cells in our study. Yadav R R et al. reported that agger nasi cells was the commonest (75.8 %) variation.12 It was found to be the 2nd common variation with prevalence of 70.6% in a study conducted by Shipilberg et al. 9 Anitha Christina Mathuram, Senthil Kumar Aiyappan et al. reported that there was no statistical correlation which corresponded to our study.13 However Espinosa W et al. and Kaya M et al. showed statistically significant relationship between agger nasi cells and sinusitis. 14, 15
The second common variation was nasal septal spur which constituted 48.8% (61 out of 125). We found that the spur was most common on the left side. Minimal or no sinusitis was seen in 14 (22.95%) and moderate to significant sinusitis was present in 47 (77.05%) patients with significant p value (0.027). Hence significant correlation was found between the sinusitis and nasal septal spur. Kaya M et al. found that 8.2% of the patients were having septal spur without any significant association with sinusitis. 15
The third common variation was ethmoid bullosa which constituted 48% (60 out of 125). Among them 83.33% were bilateral and 16.67% were unilateral (70% of them were present on the right side). Moderate to significant sinusitis was present in 45 (75%) patients with insignificant p value (0.13). Hence no significant correlation was found. Kaya M et al. found that 46.9% of patient with ethmoid bullosa was having sinusitis without any significant association. 15
The fourth common variation was supra-orbital cells which constituted 41.6% (52 out of 125). Among them 76.92 % were bilateral and 23.08 % were unilateral (75% of them were present on the left side). Moderate to significant sinusitis was present in 43 (82.69%) patients with insignificant p value (0.12). Hence no significant correlation was found between the sinusitis and supra-orbital cells. Nouraei SA showed the incidence of supraorbital ethmoid cell was 6% and it posed significant postoperative complications {immediate post-operative complications (orbital hematoma, CSF leak, meningitis) as well as late post post-operative complications (meningocoele, lacrimal duct injury)}, if not evaluated pre-operatively. 10, 16
The fifth common variation was deviated nasal septum which constituted 40% (50 out of 125). Commonest type was S-shaped, followed by C-shaped and then reversed-C shaped. Range of septal deviation was from 3 mm to 11.2 mm. Minimal or no sinusitis was seen in 8 (16%) and moderate to significant sinusitis was present in 42 (84%) patients with significant p value (0.049). Hence significant correlation was found between the sinusitis and deviated nasal septum. Studies conducted by Anitha Christina Mathuram, Senthil Kumar Aiyappan et al. in 2019, Gupta S et al. in 2016 and Devareddy et al. showed that DNS was the commonest variation detected by CT scan.13, 17, 18 Espinosa W et al. showed a statistically significant relationship between deviated septum with sinusitis which was in favour of our study. 14
These discrepancies of associations of sinusitis with various anatomical variation of paranasal sinuses between our study and other authors may be due to difference in the demographic profile of the study population along with inflammation of the drainage pathway leading to stenosis.
Limitations
The association of different anatomic variations of PNS with one another was not analysed. Patients were divided into 2 groups, one with no or minimal mucosal thickening and another with moderate to severe mucosal thickening. It had been observed that patients with clinically significant sinusitis had no or minimal mucosal thickening on CT scan. It could be due to the patient might have had significant sinusitis at the time of presentation to hospital and which could have resolved at the imaging due to time lag. The study had been done on a small population size.
Conclusions
Statistically significant correlation was found between the sinusitis & nasal septal spur and between sinusitis & deviated nasal septum in our study. Rest of the PNS variations didn’t show statistically significant correlation. So, we conclude that certain types of paranasal sinus variations may increase the risk of developing sinusitis due to obstructing the drainage pathway. Clinical evaluation of the disease should be of prime importance and if the patient is not responding significantly to the treatment, then CT should complement it to rule out surgical causes. So, for the pre-operative assessment, MDCT is the modality of choice to identify anatomical variations of the paranasal sinuses.
Abbreviations
-
PNS - Paranasal sinuses
-
CT - Computed Tomography
-
OMC - Osteomeatal complex
-
HRCT - High resolution CT
-
IEC - Institutional Ethical Committee
-
PACS - Picture archiving and communicating system
-
DNS - Deviated nasal septum
Disclosure
Competing interests: None.
Funding: None.
Author’s Contribution: Manisha Kumari- image interpretation, statistical analysis & literature search, Govind Kumar– conceptualization and design, Vinod Kumar - literature search and manuscript preparation, Sanjay Kumar Suman –image interpretation and editing, Sarita Mishra– manuscript review.
Acknowledgement: We are thankful to our staff and technicians for their valuable effort to make this study complete. We also want to thank Dr Shishir for his significant contribution on statistical analysis of the patient data.