

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.v11.i1.24.91
Year: 2025, Volume: 11, Issue: 1, Pages: 26-31
Original Article
B P Preethi1 , D B Shubha2 , Suresh Babu3
1Professor, Department of Biochemistry, Member & Resource person, Medical Education Unit, J J M Medical College, MCC B Block, Davangere, 577004, Karnataka, India,
2Associate Professor, Department of Community Medicine, Resource person, Medical Education Unit, J J M Medical College, MCC B Block, Davangere, 577004, Karnataka, India,
3Professor, Department of Biochemistry, J J M Medical College, MCC B Block, Davangere, 577004, Karnataka, India
Address for correspondence:
B P Preethi, Professor, Department of Biochemistry, Member & Resource person, Medical Education Unit, J J M Medical College, MCC B Block, Davangere, 577004, Karnataka, India.
E-mail: [email protected]
Received Date:22 March 2024, Accepted Date:03 January 2025, Published Date:06 February 2025
Introduction: CBME being implemented requires students to engage reflectively. Here students are required to describe what they have learned from a given situation/scenario, interpret it and its future application. It is observed that reflective writing is not being used for professional development, many times it is copied and pasted from peers. This initiated us to incorporate elements of assessment and constructive feedback to facilitate students to use reflective writing as Professional development tool. Materials and methods: This was an interventional study where students' reflections following ECE and AETCOM sessions were assessed using REFLECT rubric by faculty followed by feedback. Effectiveness of intervention was evaluated using Kirkpatrick model, level 1 by obtaining students' and faculty perceptions, level 2 by grading their reflections. Results: 72 (90%) of students' reflections were in level 1 after first session. With five cyclic reinforcements, 58 (72.5%) progressed to level 3 of true reflection, 4(5%) advanced to level 4 of critical reflection,14 (17.5%) attained level 2 of introspection, only 4(5%) remained in level 1. Both students and faculty perceived that repeated exposures facilitated in-depth understanding and critical analysis of clinical encounters, and internalization of attributes such as professionalism, ethics, empathy, compassion, communication skills. Conclusion: Reflective writing skills are not inherent can be acquired with experiential learning complemented with assessments and feedback. Multiple reinforcements of reflections following ECE and AETCOM sessions facilitated students to internalize clinical reasoning and decision-making skills and sensitized them to professionalism, ethics, empathy, compassion, and basic communication skills thereby contributing to their Professional development.
Keywords: Reflective writing, Assessment, REFLECT, Medical students
Reflection is a metacognitive process that creates a greater understanding of both the self and the situation so that future actions can be informed by this understanding. Self-regulated and lifelong learning have reflection as an essential aspect, and it is also required to develop both a therapeutic relationship and professional expertise. 1 There are a variety of educational approaches in undergraduate, postgraduate, and continuing medical education that can be used to facilitate reflection, from text-based reflective journals and critical incident reports to the creative use of digital media and storytelling. The choice of approach varies with the intended outcomes, but it should also be determined by the user since everyone has a preferred style. Guided reflection, with a supportive challenge from a mentor or facilitator, is important so that underlying assumptions can be challenged, and new perspectives considered. Feedback also has an important role in enhancing reflection. 2 There is little research evidence to suggest that reflection improves quality of care, but the process of care can be enhanced.
Competency-based medical education being implemented requires students to engage reflectively. Reflection is a process of exploration and explanation of events in the form of description, interpretation, and outcome. Here students are required to describe what they have learned from the given situation/scenario, interpret it and how will they apply that context in the future. In our institution, students are required to undertake reflective writing as a part of ECE early clinical exposure and AETCOM Attitude ethics and communication sessions. What has been observed of our students is that reflective writing is not being used for professional development, many times it is copied and pasted from their peers. This initiated us to incorporate elements of assessment and constructive feedback for each student’s reflection to facilitate students to use reflective writing as a Professional development tool.
This was an interventional study conducted in two phases with pilot implementation followed by full-fledged implementation among phase 1 medical students of a private medical college in central Karnataka after obtaining Institutional ethical committee clearance. The intervention used was the assessment of reflections of students using the REFLECT rubric (Figure 1) by faculty followed by feedback. Program evaluation was done using Kirkpatrick’s evaluation model. Kirkpatrick’s Level 1 evaluation was done using a perception questionnaire designed by authors and validated by subject experts. The internal consistency of questionnaire calculated using Cronbach’s alpha was 0.96. Kirkpatrick’s Level 2 evaluation was done by assessing reflections using the REFLECT rubric. 2

Training phase: Two different workshops were conducted to train students and faculty. Students were sensitized through the workshop towards the importance of reflective writing, how to critically reflect, and the tool that will be used for assessing their reflective writing. Students were trained to write reflections using Borton’s model which consisted of three components for describing their reflections in the form; of What happened? So what? And what next? A separate workshop was conducted for faculty to train them in assessing reflections using the REFLECT rubric. This rubric is comprised of 4 levels; level 1 is No reflection, level 2 is Introspection, level 3 is actual reflection and level 4 is critical reflection. The context for reflections were: ECE early clinical exposure and AETCOM sessions (5 encounters: 4 ECE encounters on clinical reasoning & decision-making skills, one AETCOM session on effective communication skills, ethics & professionalism, empathy & compassion covering all aspects of professional development). ECE sessions were conducted as follows: briefing about the basic science aspect of clinical cases by faculty followed by hospital visits and reflections by students and its documentation in the logbook and lastly summarization by faculty. AETCOM sessions were conducted using role plays to impart various attributes of clinicians as professional, empathetic, compassionate, ethical, and effective communication skills.
This was followed by students writing reflections and faculty feedback.
Implementation phase: pilot implementation on 10 students and these were not included in the results of the main study. Faculty instructed students to engage in reflective writing during ECE and AETCOM sessions and document it in the logbook. Assessment of reflections was done by faculty using the REFLECT rubric. Faculty identified to which level of reflection each student belongs and feedback was provided regarding how to indulge in critical reflection. Students' and faculty's perceptions were obtained using a questionnaire administered through Google Forms.
Out of 125 students, 10 participated in the pilot study and these were excluded from the main analysis. From the remaining 115 students, 80 completed all 5 encounters which included 4 ECE sessions and one AETCOM session and 35 were excluded from analysis who failed to complete all five encounters.
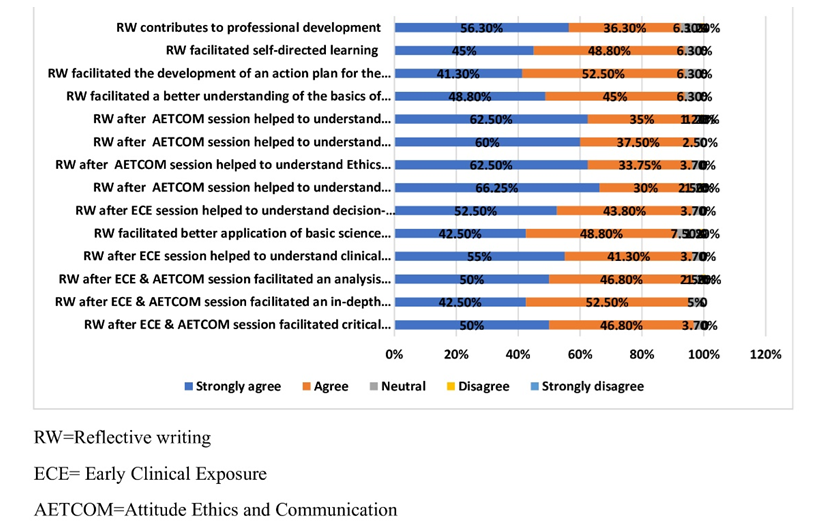
More than 90% of our students agreed that at the end of five encounters, guided reflective writing facilitated critical thinking, a better and more in-depth understanding of ECE and AETCOM sessions, and their ability to analyze the same. This is because reflecting after each session/encounter stimulated exploratory interactions of their thoughts. All of them perceived that they were able to indulge in effective clinical reasoning and decision-making. Reflecting on ECE sessions helped students bridge the gap between knowledge acquisition of basic sciences and their application. Further, these sessions when reinforced multiple times improved their clinical reasoning and decision making. Most of them opined that they were able to appreciate and understand professionalism, ethics, empathy, and compassion after attending and reflecting on the AETCOM session. Role plays with right and wrong versions helped students to understand the basics of effective communication skills and appreciate attributes of thorough clinicians as professional, ethical, empathetic, and compassionate. Most of our students agreed that with repetitive reflective writing, they were able to develop action plans for their future clinical practice. These guided and graded reflective writing facilitated self-directed learning among students and contributed towards their professional development. However, around 1.2% to 7.5% of students were neutral in their responses (Figure 2). These students were passive in their approach towards these ECE and AETCOM sessions and were found to be poor reflectors after the assessment of their reflective writing.
100% of faculty perceived that reflective writing by students, its assessment, and feedback by faculty facilitated critical thinking, thoughtful introspections, and the ability to analyze situations among phase 1 medical students. They also agreed that these activities stimulated students to explore their values, beliefs, conflicts, and their impact on their personality. All the faulty agreed reflective writing by students, its assessment, and feedback by faculty is very much needed so that it can be used as a professional development tool. However, 14.3% of faculty were neutral in their responses and another 14.3% disagreed with the assessment and feedback as it demanded little extra time when compared to their routine teaching activities (Figure 3).

Students' reflective writing after each ECE and AETCOM session was assessed by faculty using the REFLECT rubric and grading of students' reflections was done based on their reflective capacity as level 1/no true reflection, level 2/thorough introspection, level 3/appropriate reflection, and level 4/critical reflection. At the end of 1st ECE session, 70 (90%) students were in level 1 and 8 (10%) in level 2 with no candidates having level 3 and level 4 reflective capacity indicating that most of the students were novices in their reflective writing with just casual description of ECE encounter. At the end of the 2nd ECE session, 50 (62.5%) students were in level 1 and 30 (37.5%) in level 2 amounting to 22 students progressing towards thoughtful introspection ie attaining level 2. Guided reflective writing with assessment and feedback by faculty facilitated these 22 students towards the next immediate level. At the end of the 3rd ECE session, 24 (30%) students were in level 1, 46 (57.5%) in level 2 and 10 (25%) in level 3. This accounted for 26 students progressing to level 2 from level 1 and 10 students progressing to level 3 from level 2. Repetitive exposure played an important role in helping students attain progression in their reflective capacity. At the end of the 4th ECE session 22.5 (18%) students were in level 1, 42 (52.5%) in level 2, and 20 (25%) in level 3. With the continued assessment of reflective writing and feedback, 4 students further progressed to level 2 from level 1 and quite a good number of 20 students progressed to level 3 indicating true reflections in their descriptions. At the end of the last AETCOM session only 4 (5%) students were in level 1, 14 (17.5%) in level 2, 58 (72.5%) in level 3, and 4 (5%) in level 4 (Table 1). Cyclic reinforcements of reflective writing by students and their assessment followed by feedback by faculty facilitated our students to advance further in their reflective capacity. We observed that, at the end of all 5 sessions only 4 students remained in level 1 when compared to 72 students during session 1, 14 students progressed to level 2 from level 1 and 38 students progressed to level 3 from level 2 and 4 students were able to achieve highest level of 4 indicating that they were able to attain critical reflecting skills (Figure 4).

|
Sessions |
Level 1 |
Level 2 |
Level 3 |
Level 4 |
|
1st ECE session |
72 (90%) |
8 (10%) |
0 |
0 |
|
2nd ECE session |
50 (62.5%) |
30 (37.5%) |
0 |
0 |
|
3rd ECE session |
24 (30%) |
46 (57.5%) |
10 (12.5%) |
0 |
|
4th ECE session |
18 (22.5%) |
42 (52.5%) |
20 (25%) |
0 |
|
5th AETCOM session |
4 (5%) |
14 (17.5%) |
58 (72.5%) |
4 (5%) |
Reflection means a process in which a person’s thoughts that are related to experiences can be decomposed and interpreted to make awareness. Thus, the created understanding in this process can be used in the future. 3 One of the methods of teaching reflection is reflective writing. With the implementation of CBME Competency-Based Medical Education, reflective writing has been included as part of ECE and AETCOM sessions for the phase 1 medical curriculum. Most of our students lacked critical reflections. Our team addressed this issue by incorporating a component of assessment of reflections using the REFLECT rubric as it’s a known fact that assessment drives learning for students. Another unique feature of our educational scholarship is that the assessment of reflections was followed by feedback from faculty to promote reflective writing as a professional development tool.
We observed incremental progression of critical reflections towards the end of five sessions of ECE and AETCOM among phase 1 medical students (Figure 4). At the end of the first ECE session, 90% of our students were in level 1 with poor reflective capacity and at the end of all five sessions, only 5% of students remained in level 1 with 14% progressing to the next level of thoughtful introspection and a maximum of 58% students advancing to level 3 with true reflections and 5% attaining the level 4 of critical reflections. Our results suggest that reflective writing among medical students need not be intuitive. They can be trained in a longitudinal program providing ample opportunities to make them competent towards critical reflection. Our observations are per that of Patterson et al who used the REFLECT rubric to analyze their student's narratives and they observed that reflective writing skills improved in 50% of their students with repeated exposures. 4 Our results are in alignment with that of Kadam et al who reported that it is possible to provide students an opportunity to practice writing reflections and gradually improve their reflective skills through continuous formative assessment. Kadam and team concluded that 65% of their students were in level1 at the end of the first session of reflective writing and at the end of the fourth session, 55% progressed to level 3. 5
At the end of all five sessions, only 5% of our students advanced towards critical reflective capacity reaching level 4. The extent to which a student goes into deeper reflection depends on their reflective capacity but with continuous formative reinforcements, students can be transformed as critical reflectors. Dekker et al 6 reported different abilities of students' reflection and grading of reflections are needed to make them competent. Further repeated exposures and constructive feedback from mentors may inculcate deep reflecting skills leading to more fruitful transformative learning among students as observed by Vasudha et al. 7
Our students perceived that reflective writing facilitated optimal critical thinking, in-depth understanding, and analysis of ECE encounters. Further, these students also opined that their clinical reasoning and sensitization towards decision-making skills improved a lot with repeated exposures. Our observations follow that of Mori et al who believe that reflective writing and faculty feedback have a positive impact on students' learning skills. 8 After participating and reflecting on AETCOM sessions, our students expressed that they were sensitized toward professionalism and, the importance of being ethical, empathetic, and compassionate. We share our observations with those of several studies 9, 10, 11 wherein it is emphasized that teaching reflections through writing can make a significant improvement in self-awareness, professionalism, and humanism and also help students learn empathy and promote compassion. Our students opined that reflective writing stimulated exploratory interactions with their thought processes and at the end of all reflections, they were able to develop action plans for their future. Coulehan agrees stating in a commentary that critical analysis and evaluation of learning experiences by students leads to new understanding and appreciation of the way they think and operate in clinical settings. 12 Further our students expressed that repeated reinforcements of reflective writing with assessment and feedback facilitated comprehensive analysis of ECE and AETCOM sessions, sensitized them towards appropriate clinical practice, and facilitated them towards the development of action plans for the future thereby contributing towards their professional development (Figure 2). Swathi Tikare 13 has reported that reflective writing is a metacognitive process that creates a greater understanding of self and situation and prepares them for informed future action.
There was good alignment in the perception of faculty with that of students in our educational scholarship. Our faculty perceived that repetitive exposures of students to reflective writing followed by grading with the REFLECT rubric help us to differentiate narratives with mere habitual action from critical reflection in an objective way and timely feedback shared with students will facilitate them to progress towards higher levels of reflections. Faculty believe that repetitive cycles of reflective writing stimulate critical thinking, thoughtful introspection, and exploration of values, beliefs, and conflicts and help them develop action plans for the future and thereby promote their professional development (Figure 3). These observations follow that of Swathi 13 and Singh et al 14 who have reported that reflective writing helps to develop skills that will be needed in future professional life for dealing with multifaceted problems. Further Daryazadeh 15 in their study emphasized teaching students to reflect improves their clinical and ethical decision-making, and problem-solving capacity, and also promotes professionalism. Using the REFLECT rubric for assessment of reflections followed by feedback can be effective in the professional development of students.
Reflective writing skills are not inherent to students. These skills can be acquired with experiential learning when complemented with assessments and feedback. It’s a known fact that assessment drives learning among students and our team did the right thing by including a component of assessment and feedback to facilitate critical reflective capacity among phase 1 medical students. Multiple reinforcements of reflections following ECE and AETCOM sessions facilitated students to internalize clinical reasoning and decision-making skills and sensitized them to professionalism, ethics, empathy, compassion, and basic of communication skills thereby contributing to their professional development.
Nil
Nil
We extend humble gratitude to ACME Faculties JNMC Nodal Center Belagavi for their constant support in completing this educational scholarship. We are thankful to our phase 1 medical students JJMMC, Davangere for participating in this project.
Subscribe now for latest articles and news.