

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.v11.i3.25.127
Year: 2025, Volume: 11, Issue: 3, Pages: 297-304
Original Article
Swathi Samalla1 , Dinesh Kasturi1 , S P Smitha Vadana1 , Aishwarya Jawalkar2
1Assistant Professor, Department of Pathology, Government Medical College and Hospital, Nizamabad, 503001, Telangana, India,
2Senior Resident, Department of Pathology, Government Medical College and Hospital, Nizamabad, 503001, Telangana, India
Address for correspondence: Aishwarya Jawalkar, Senior Resident, Department of Pathology, Government Medical College and Hospital, Nizamabad, 503001, Telangana, India.
E-mail: [email protected]
Received Date:06 April 2025, Accepted Date:14 June 2025, Published Date:14 November 2025
Introduction: Ovarian cancer is the fifth leading cause of cancer-related death in U.S. women, accounting for 3% of female cancers globally. In India, it is the third most common cancer among women, constituting 6% of cases. Histopathological examination is crucial for diagnosing ovarian tumors, as clinical and gross features alone are insufficient. Known risk factors include age, family history, nulliparity, hormone replacement therapy, and lifestyle factors. Approximately 80% of ovarian tumors are benign, occurring in women aged 20-45, while malignant tumors, with a poor prognosis, affect older women aged 40-70.This study aims to evaluate the occurrence and characteristics of both non-neoplastic and neoplastic lesions in ovarian specimens, focusing on gross and histomorphological features.
Material and methods: This retrospective study conducted at Government Medical College, Nizamabad, spanning July 2021 to July 2023, analyzed 106 ovarian lesion cases from patients undergoing cystectomy or salpingo-oophorectomy. The research involved detailed clinical and histopathological examinations, focusing on gross features and microscopic analysis to identify tumor types and relevant details.
Results: Of 106 cases, 12 were non-neoplastic lesions, 18 were tumor-like lesions and 76 were neoplastic lesions. Among neoplastic lesions, 71 cases (93.4%) were benign, 1 (1.3%) were borderline, while 4 (5.3%) cases were malignant. Histopathologically, surface epithelial tumors (82.9%) were the most common subtype followed by germ cell tumors (15.8%) and then sex cord tumors (1.3%). The most common neoplastic lesion was serous cystadenoma. Benign tumors were most common in the 21-30 years age group, while malignant tumors were most common in the 41-50 years age group. Bilaterality was seen in 9 (11.8%) of 76 gross specimens of ovarian tumors.
Conclusion: Ovarian neoplasms exhibit diverse clinicomorphological features, with surface epithelial tumors being the most common and often affecting reproductive age groups. While advancements like immunohistochemistry and genetic studies enhance precision, histopathological examination remains the gold standard for diagnosis and prognostic evaluation, especially in resource-limited institutes.
Ovarian cancer accounts for 3% of all cancers in females and is the fifth most common cause of death due to cancer in women in the United States 1, with an estimated 313,959 new cases and 207,252 deaths worldwide 2. According to the Global Cancer Observatory (GLOBOCAN) 2018, the age-standardized incidence rate for India is 3.8-5.5 cases per 100,000 females per year 3. National Cancer Registry Programmed (NCRP) states that ovarian cancer is the third most common cancer among Indian women after breast and cervix cancer and constitutes about 6% of total cancer cases among Indian women 4.
A wide spectrum of pathological conditions which are non-neoplastic and neoplastic can be seen in the ovary in routine surgical pathology 5. Ovarian neoplasms should be differentiated from non-neoplastic functional cysts as they can be treated with minimal intervention 6. Primary ovarian tumors can arise from one of three ovarian components: surface epithelium, germ cells, and ovarian stromal cells including the sex cords. Surface epithelial tumors constitute the majority of ovarian neoplasms. Most ovarian tumors cannot be differentiated based on clinical and gross features alone, hence histopathological examination is important for diagnosing ovarian tumors and it plays an important role in determining treatment and prognosis. Because most ovarian cancers have spread beyond the ovary and fallopian tube by the time of diagnosis, they account for a large number of deaths from cancer of the female genital tract 1.
Despite the high incidence and mortality rates, the etiology of ovarian cancers is poorly understood. Established risk factors for ovarian cancer include age, family history of ovarian cancer, nulliparity. Other possible risk factors include postmenopausal hormone replacement therapy and lifestyle factors such as cigarette smoking, alcohol consumption and obesity 7.
About 80% of ovarian tumors are benign and occur between ages of 20 to 45 years whereas 20% of ovarian tumors are malignant and commonly occur in older women between ages of 40 to 70 years with poor prognosis 8, 9.
Tumor stage and laterality may also indicate the nature of the tumor. While sex cord stromal tumors are predominantly confined to a single ovary, bilateral ovarian tumors are commonly seen in serous carcinoma and tumors which metastasize to ovary 10.
This study contributes to existing literature by highlighting both common and rare ovarian tumors, including clear cell carcinoma, yolk sac tumor, and juvenile granulosa cell tumor. Reporting these rare entities from a resource-limited tertiary center offers region-specific insights that may improve diagnostic and clinical decision-making.
The aim of this study is
To assess the frequency of non-neoplastic and neoplastic lesions in ovarian specimens in our institute
To study the gross and Histomorphological features of various ovarian lesions.
The present study was a retrospective (observational) study carried out in the Department of Pathology, Government General Hospital, Nizamabad over a period of 2 years from July 2021 to July 2023. A total of 106 cases of ovarian lesions were studied for patients who underwent unilateral/bilateral ovarian cystectomy or salpingo-oophorectomy with total abdominal hysterectomy. Normal ovaries were excluded from the study. The ethical clearance was granted by Government medical college, Nizamabad, Telangana.
Information regarding the age of the patient, detailed clinical history was obtained from the patients. The ovarian specimens were fixed in 10% neutral buffered formalin.
Gross examination was done visualizing the outer surface and cut surface looking for cyst, locularity, type of cystic fluid, any solid areas, granular concretions, hemorrhage, or necrosis.
After fixation for 24 to 48 hours, sections were given from representative areas and were processed by routine histopathological procedure, stained with hematoxylin and eosin staining followed by microscopic examination. The data obtained after microscopy included information about type of tumor and other relevant details. In cases where histomorphological features were insufficient for definitive classification, immunohistochemistry was employed externally at a higher referral center, considering the limitations in in-house IHC facilities.
The data were entered into an Excel sheet and further analysis was done using IBM statistical package for social sciences (SPSS) for Windows to assay the frequencies and percentages of all variables that were documented.
An observational study was conducted and a total of 106 cases of ovarian lesions were assessed over a period of 2 years (July 2021- July 2023) of which neoplastic and non-neoplastic lesions were identified. Of 106 cases, 12 were non-neoplastic lesions, 18 were tumor-like lesions and 76 were neoplastic lesions. Tumor-like ovarian lesions includes 5 cases (16.7%) of corpus luteal cysts, 13 cases (43.3%) of follicular cysts. Among 12 cases of non-neoplastic lesions, all cases were of Hemorrhagic Cyst secondary to torsion. They were seen within the 11-40 years age group.
Among 18 cases of tumor-like lesions, 5 were luteal Cysts and 13 were follicular Cysts. They were seen within the 21-50 age group with maximum incidence in the 31-40 age group.
Among neoplastic lesions, the maximum number of patients were in their third decade of life and the distribution of the cases was within the age range of 11-70 years. The majority of cases of benign tumors were seen in the 21-30 years age group, borderline tumors in the 61-70 years age group and malignant tumors in the 41–50-year age group. The youngest patient was a 12-year female with serous cystadenoma with torsion and the oldest patient was 70 years female with Borderline Mucinous tumor.
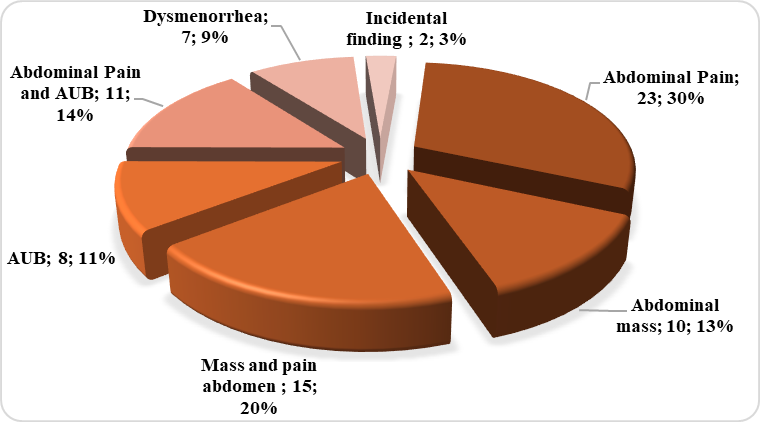
The most common presentation of ovarian neoplasms was abdominal pain seen in 23 (30.3%) cases followed by mass and heaviness of abdomen with pain in 15 (19.7%) cases & abdominal pain with abnormal uterine bleeding in 11 (14.5%) cases (Figure 1).
Out of 76 cases of ovarian neoplasms, 71 (93.4%) cases were benign, 1 (1.3%) was borderline while 4 (5.3%) cases were malignant.
Gross examination of the specimens revealed that most of the tumors were cystic in 56(73.7%) cases followed by mixed (cystic with solid component) in 20(26.3%) cases. Majority of the benign lesions (56 cases: 73.7%) were cystic in consistency while few cases (15 cases: 19.7%) had both solid and cystic consistency. All cases of borderline group and malignant cases were mixed in consistency.
Based on the site of involvement, the majority of the tumors were unilateral 67(88.1%) cases. Involvement of the left ovary (36 cases: 47.4%) was more common than the right (31 cases: 40.8%). Bilaterality was seen in 9 (11.8%) cases. The bilateral tumors were serous cystadenoma (6 cases), mature cystic teratoma (2 cases) and mucinous cystadenoma (1 case).
Histopathologically, surface epithelial tumors constituted the majority of the ovarian neoplasms with 63 (82.9%) cases, followed by germ cell tumors which constituted 12(15.8%) cases; sex cord stromal tumors were seen in one (1.3%) case (Table 1).
|
Histopath- ological Diagnosis |
Nature of Tumor |
Types |
Number of Cases (N=76) |
Percentage (%) |
|
Surface Epithelial Neoplasms |
Benign |
Serous cystadenoma |
46 |
60.6 |
|
Mucinous cystadenoma |
11 |
14.5 |
||
|
Serous cystadenofibroma |
2 |
2.6 |
||
|
Mucinous Cystadenofibroma |
1 |
1.3 |
||
|
Borderline |
Borderline Mucinous tumor |
1 |
1.3 |
|
|
Malignant |
Mucinous cystadenocarcinoma |
1 |
1.3 |
|
|
Clear cell carcinoma |
1 |
1.3 |
||
|
Germ cell tumor |
Benign |
Teratoma benign |
11 |
14.5 |
|
Malignant |
Yolk sac tumor |
1 |
1.3 |
|
|
Sex cord Stromal tumor |
Malignant |
Juvenile granulosa cell tumor |
1 |
1.3 |
|
Total |
76 |
100% |
||
Among benign tumors, serous cystadenoma was seen in the maximum number of cases constituting 60.6% (46 cases) of the total cases followed by mucinous cystadenoma (11 cases: 14.5%) and mature cystic teratoma (11 cases: 14.5%).
Among borderline tumors, 1 case of Mucinous borderline tumor was seen.
Among malignant tumors, Mucinous adenocarcinoma (1 case), Clear cell carcinoma (1 case), yolk sac tumor (1 case) and juvenile granulosa cell tumor (1 case) were seen.
Ovarian tumors are notorious silent killers as they escape attention in the early stage due to their anatomical location, present with vague clinical symptoms like mass, pain in the abdomen, abdominal distension and are often not noticed until they have achieved a huge size 11. Ovarian tumors represent a range of pathology from benign mass through tumors of borderline malignant potential to invasive cancers. Diagnosis at an early stage is extremely important but remains a challenge 12. Due to monthly hormonal and traumatic insults during ovulatory cycles, they are more prone to mutations resulting in tumorigenesis 13. Histomorphological classification is important in the evaluation of ovarian neoplasms.
In the current study, a total of 106 cases of ovarian lesions were studied. Out of which 76 (71.7%) cases were of ovarian tumors and 30 (28.3%) cases were of tumor-like ovarian lesions. Follicular Cysts were more common than luteal Cysts.
Of 76 neoplastic lesions, 71 cases (93.4%) were benign, 1 (1.3%) was borderline, while 4 (5.3%) cases were malignant. Our findings are consistent with the studies done by Patel et al., 14 Wills V, et al., 15. Almost similar results were seen in many different studies where benign tumors were more common than malignant tumors 16, 17, 18 (Table 2, Table 3).
Ovarian tumors were classified according to WHO classification. Among the different histopathological patterns, Surface epithelial tumors constituted the majority of ovarian neoplasms with 63 cases (82.9%), followed by Germ cell tumors of 12 cases (15.8%) and sex cord-stromal tumors in 1 case (1.3%) which was correlating with other studies. Metastatic tumor was not found in the present study.
In this study, serous tumors constituted 66.2% (48 cases) of all ovarian tumors consistent with findings of Mehra P et al. with 55.5%19 and Patel et al.14 with 58.7%. Mucinous tumors comprised 17% (13 cases) of all ovarian tumors similar to findings of Patel et al.14 with 18.5%.
Among the serous tumors, serous cystadenoma constituting 60.6% (46 cases) was the most common benign tumor similar to findings of Patel et al.14 with 57.4% of cases and serous cystadenofibroma cases comprised 2.6% (2 cases).
Among mucinous tumors, mucinous cystadenoma constituted 14.5% and was the second most common surface epithelial tumor, 1.3% of mucinous cystadenofibroma which was similar to results of Maheshwari V et al. 21 and Wills V et al. 15
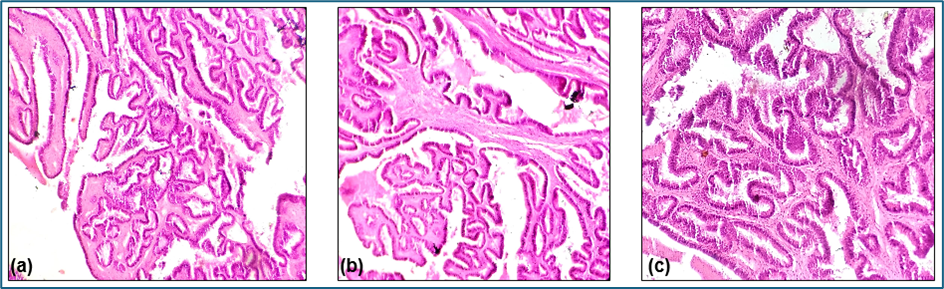
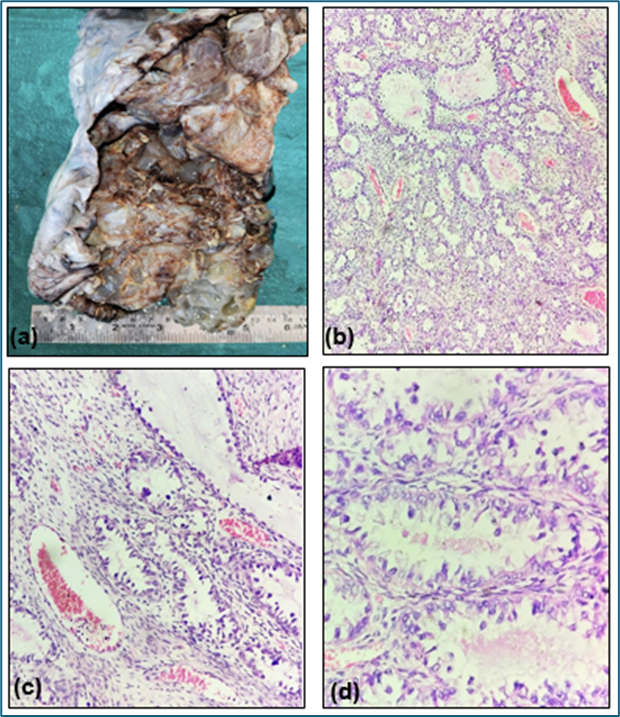
In current study, 1 case of Mucinous borderline tumor was reported in a 70-year female who presented with abdominal mass. Gross examination of the right ovary from total abdominal hysterectomy specimen revealed a large ovarian cyst measuring 12x7cms. Cut surface showed gray white solid areas along with mucin filled cystic areas. Microscopic examination revealed cyst wall lined by broad complex hierarchical branching papillae lined by cuboidal to columnar epithelium. Individual cells are large with moderate amount of cytoplasm, increased nuclear cytoplasmic ratio, vesicular nuclei with few of them showing prominent nucleoli with irregular nuclear borders. Mitotic activity seen. No frank stromal invasion noted (Figure 3).
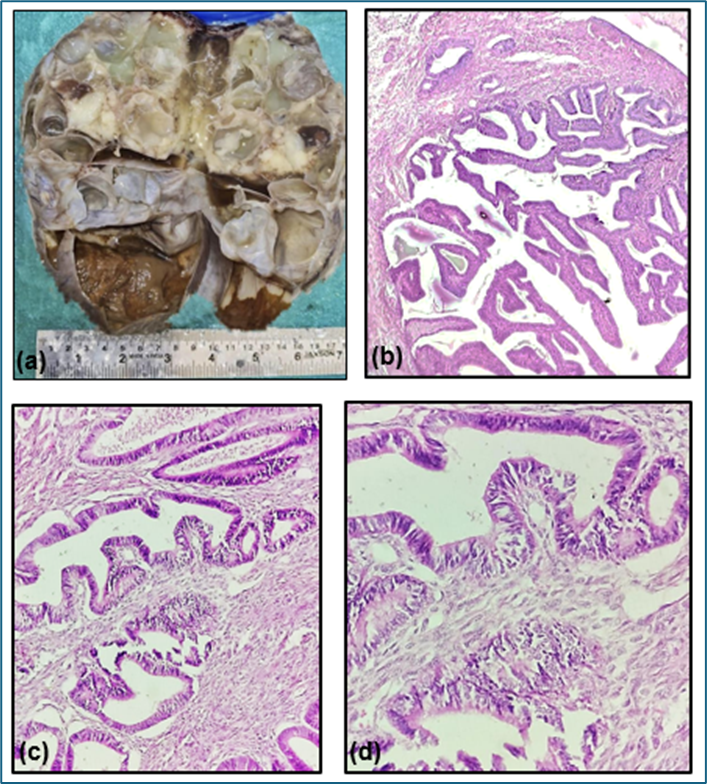
In current study, 1 case of Mucinous cystadenocarcinoma was reported in a 65-year female who presented with abdominal mass and pain. Gross examination of the right ovary specimen revealed a large ovarian cyst measuring 22x20cms. Cut surface showed solid and cystic areas. Solid areas showed papillary excrescences. Cystic areas were filled with partly mucinous and partly serous fluid.
Microscopic examination revealed cyst wall lined by large round to spindle shaped cells arranged in a papillary pattern with fibrovascular core. These cells show anisocytosis with altered nuclear cytoplasmic ratio. Capsular invasion is also noted (Figure 4).
Among Clear cell tumors, 1 case of Clear cell carcinoma was reported in a 46-year female who presented with abdominal mass, abdominal pain, and unilateral ovarian mass. Gross examination revealed a large multilocular cyst measuring 17x13cm. Cut surface shows cystic and solid areas. Cystic areas are filled with mucinous fluid with gray brown, nodular with hemorrhagic solid areas.
Microscopic examination revealed tumor tissue arranged in papillary, glandular and tubulocystic pattern lined by low cuboidal with granular eosinophilic cytoplasm and protruding nuclei: Oxyphilic cells with hobnail pattern. Few cells show clear cytoplasm with hobnail nuclei (Figure 5).
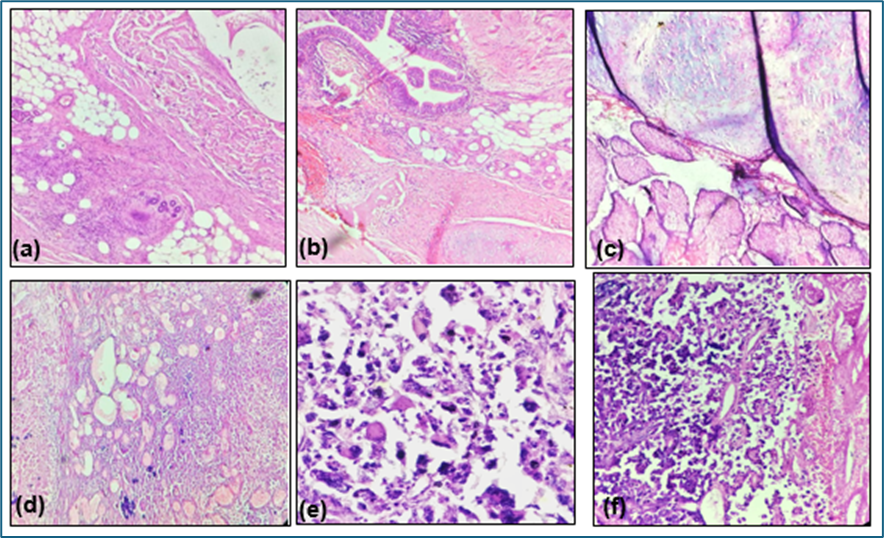
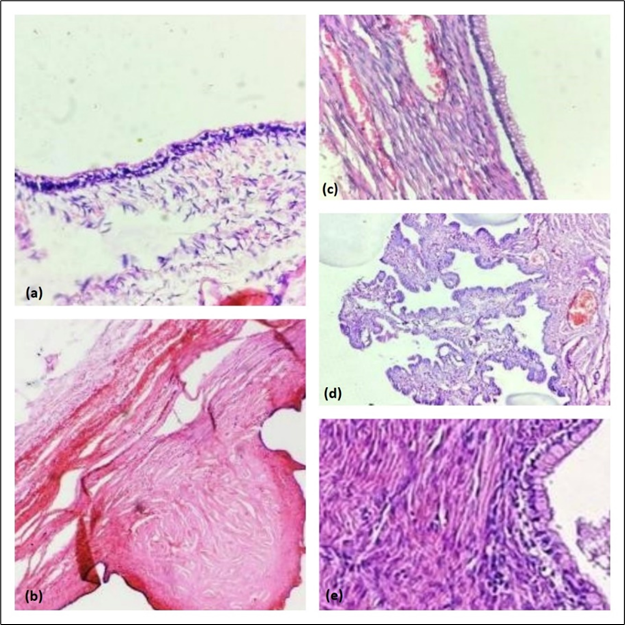
In this study germ cell tumors accounted for the second most common ovarian tumor accounting for 15.7% of all ovarian tumors. Among 12 cases of germ cell tumors, mature teratoma was the commonest about 14.5% of all ovarian tumors which is equal to mucinous cystadenoma (14.5%).
Among malignant tumors, 1 case (1.3%) of yolk sac tumor was reported during our study period in a 40-year female who presented with abdominal pain and rapidly growing mass. The gross specimen weighed 6kgs, measuring 28x22cms, smooth and glistening external surface, cystic and solid areas on cut surface with hemorrhage. Microscopic examination revealed normal ovarian stroma and tumor tissue. Tumor tissue arranged in microcystic pattern with hyaline globules and Schiller-duval bodies and focal areas of undifferentiated solid pattern with bizarre nuclei.
In the present study, we reported only 1 case of sex cord stromal cell tumor in a 27-year-old pregnant female with incidental finding of right ovarian cyst during pregnancy. Gross examination of the right ovarian cystectomy specimen revealed a large ovarian cyst measuring 20x19cms. Cut surface showed gray white to gray brown solid and cystic areas. Cystic areas were filled with mucinous fluid. Microscopic examination revealed tumor arranged in trabecular, nests and micro follicles. Tumor cells are oval/cuboidal with nuclear atypia, paucity of nuclear grooves and increased mitotic activity. Few foci of luteinized cells are seen (Figure 7).
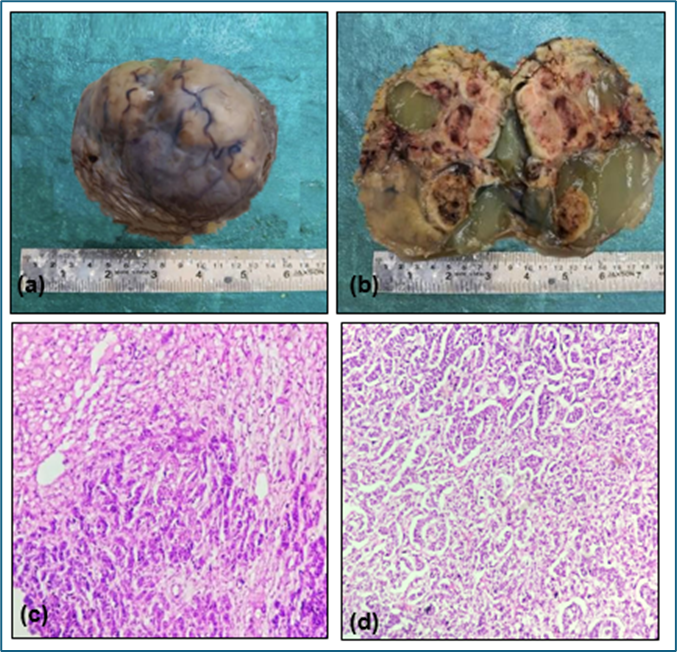
Immunohistochemistry at a higher center revealed Calretinin & CD99 Positivity and negative for cytokeratin, SF1, SALL4, Inhibin and Melan A consistent with Juvenile granulosa cell tumor.
The limitation in this study was the sample size, as larger sample size would have facilitated the classification of a greater variety of cases. Additionally, since this research was conducted at a single institution, it does not account for the prevalence of ovarian neoplasms across an entire country or state.
Ovarian Cysts and masses show a wide morphological diversity and pose many challenges. Correlation of clinical history, radiological findings, gross examination along with microscopic examination is essential for overall management and prognosis. The ovarian neoplasms in our institute represented a wide histomorphological spectrum. Benign ovarian tumors were more common than malignant and seen in all age groups with predominance in the third decade of life. Abdominal pain was the most common clinical presentation. Based on histopathology, surface epithelial tumors were most common, with serous tumors being the common variant, followed by mucinous tumors and germ cell tumors. Incidence of malignant cases were low in our study compared to other studies. Among the rare malignant tumors, Clear cell carcinoma, Yolk sac tumor and juvenile granulosa cell tumor are reported in our study. Early diagnosis is very crucial to reduce morbidity and mortality among these patients. In cases such as the juvenile granulosa cell tumor, immunohistochemistry proved vital in confirming the diagnosis, underscoring the role of ancillary techniques in challenging cases and highlighting the importance of adjunct diagnostic modalities, particularly in resource-constrained centers.
Authors acknowledge Dr. Mohd Imran Ali, Professor and HOD, Department of Pathology, Government Medical College and Hospital Nizamabad, Telangana, India.
Nil.
Authors declare no conflicts of interest.
Subscribe now for latest articles and news.