Savithri Ravindra1, Thejasvi Krishnamurthy2, V Geethamani3
1Associate Professor, Department of Pathology, Kempegowda Institute of Medical Sciences, Bengaluru, Karnataka, India, 2Assistant Professor, Department of Pathology, Kempegowda Institute of Medical Sciences, Bengaluru, Karnataka, India, 3Former Professor, Department of Pathology, Kempegowda Institute of Medical Sciences, Bengaluru, Karnataka, India
Address for correspondence:
Dr. Savithri Ravindra, Department of Pathology, Kempegowda Institute of Medical Sciences, Bengaluru - 560 070, Karnataka,
India. Phone: +91-9845133869. E-mail: [email protected]
Abstract
Pilomatrixoma is a benign skin neoplasm of hair matrix origin, commonly seen in the head and neck region. Pre-operative fine-needle aspiration cytological (FNAC) diagnosis helps in the management of the case. It is important to identify the benign neoplasm on FNA smears, as surgical excision is curative. We present a case of 21-year-old male presenting with a swelling below the ear lobe. With the clinical impression of parotid tumor/lipoma, he was referred for FNAC. On aspiration, the scant whitish material was obtained. Smears showed clusters of anucleate squamous cells, small groups of basaloid cells, many multinucleated giant cells and macrophages. Cytological diagnosis of pilomatrixoma was made, which was later confirmed by histopathology.
KEY WORDS:Cytology, fine-needle aspiration cytological, pilomatricoma
Introduction
Pilomatrixoma is a benign skin neoplasm of hair matrix origin, commonly seen in the head and neck region. It may occur in the parotid region and mimic parotid tumor clinically. There are case reports of pilomatrixoma mimicking parotid tumors.[1,2] Cozzi et al.[1] reported a case of giant pilomatrixoma mimicking malignant parotid mass clinically, where preoperative biopsy gave the correct diagnosis.
Fine-needle aspiration cytology (FNAC) plays an important role in the pre-operative diagnosis. Correct pre-operative cytological diagnosis helps in the management of the case, as surgical excision is curative.
|
Case Report
A 21-year-old male presented with a nodule below the right ear lobe. The nodule was 2 cm × 1 cm and had a smooth surface. With the clinical impression of a parotid neoplasm/lipoma in the parotid region, the case was referred for FNAC.
Aspiration was performed in the cytopathology section using 23 g needle and syringe. The aspirate was scant and whitish. Smears made and fixed in 95% alcohol and stained by Papanicolaou (Pap) and hematoxylin and eosin stain.
Microscopy The smears were cellular, showed loosely cohesive basaloid cells and anucleate squamous cells (squames) in clusters and as singles (Figure 1). Many multinucleated giant cells and scattered macrophages were noted (Figure 2). There were no nucleated squamous cells, all the cells appeared benign, did not show cytoplasmic vacuolations. Cytological diagnosis of pilomatrixoma was made.
Later the nodule was excised and sent for histopathological examination, which confirmed the diagnosis of pilomatrixoma (Figures 3 and 4).
|
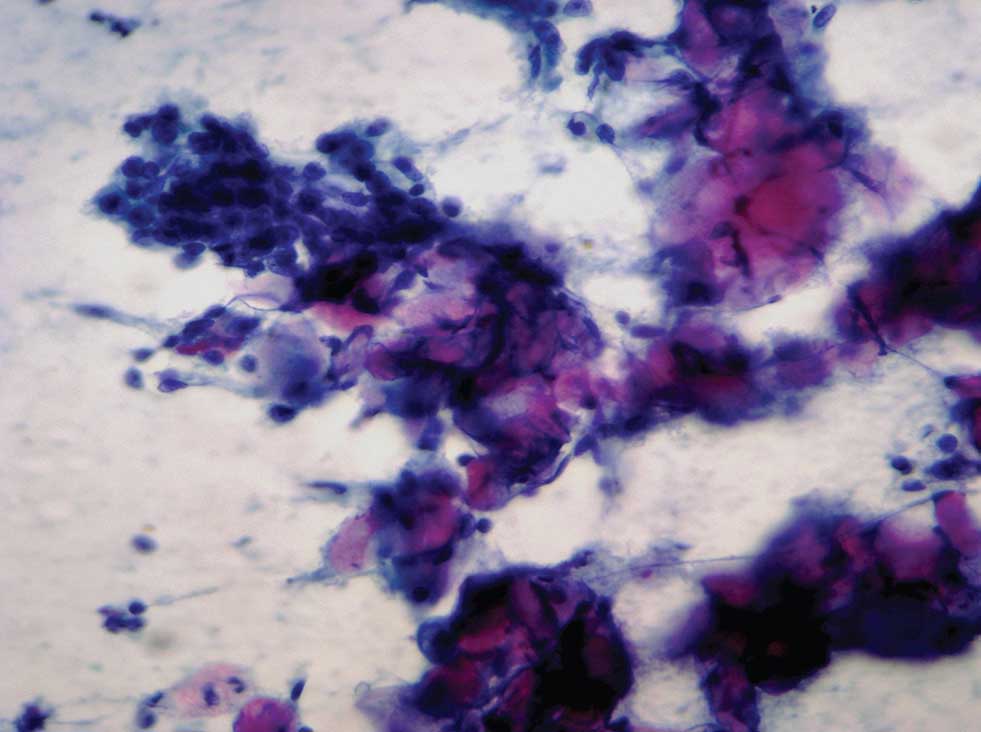 |
Figure 1: Clusters of anucleate squamous cells and basaloid cells in the smear (Pap, ×400) |
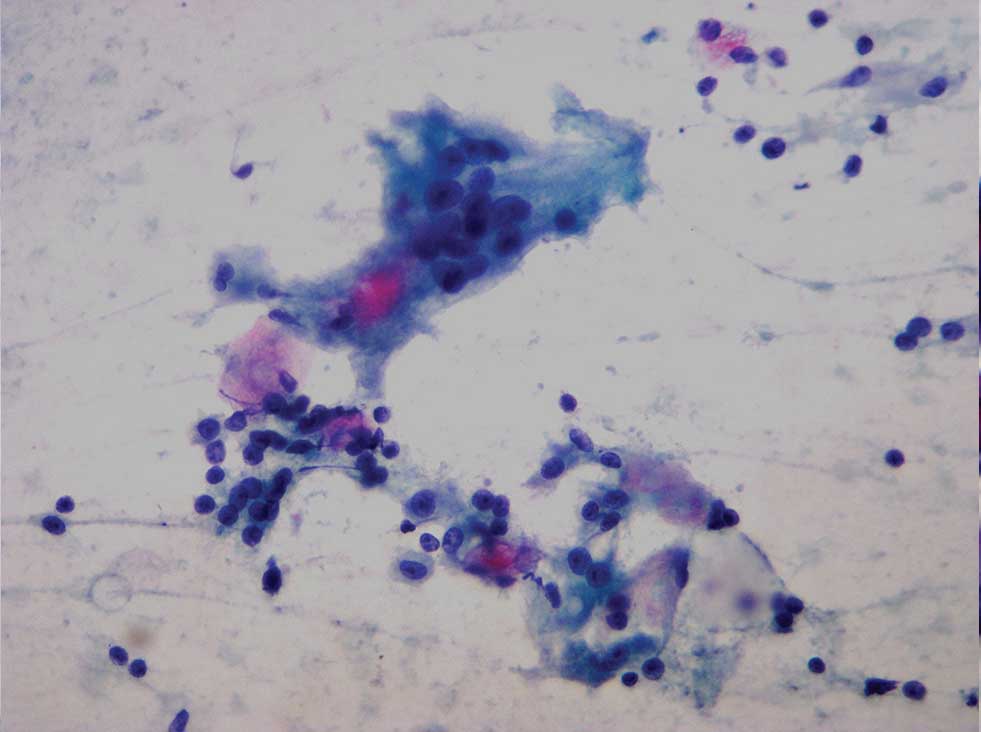 |
Figure 2: Macrophages and multinucleate giant cells along with anucleate squamous cell and basaloid cells in the smear (Pap, ×400) |
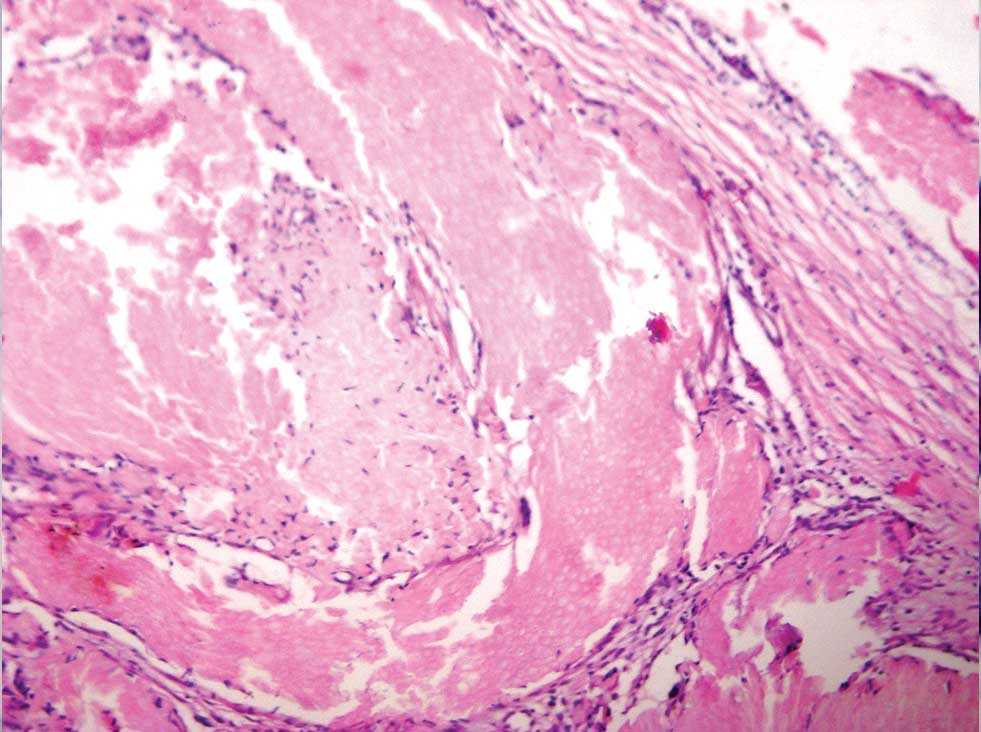 |
Figure 3: Histopathology section of pilomatrixoma (H and E, ×100) |
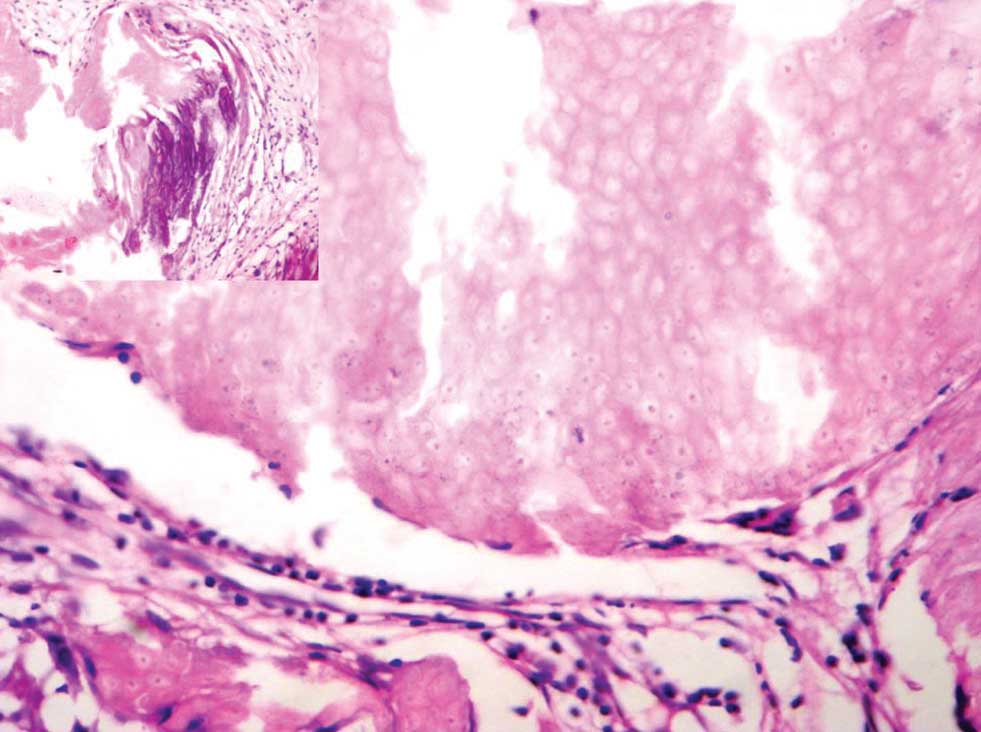 |
Figure 4: Histopathology section showing the “ghost cells” (H and E, ×400), calcification in the inset |
|
Discussion
Pilomatrixoma is a benign skin neoplasm of hair matrix origin, commonly seen in the head and neck region. One can expect it in the parotid region too, mimicking a parotid tumor. Initial cytological diagnosis plays an important role in identifying the nature of the lesion. Cytomorphology of pilomatixoma is described by many authors.[3-6] The presence of anucleate squamous cells and basaloid cells are the most common findings, and the proportion can vary. Sánchez Sánchez et al.[7] have cautioned not to over diagnose malignancy when there is the predominance of basaloid cells with nucleoli. In the present case, there were few groups of basaloid cells and anucleate squamous cells in clusters.
Pilomatrixoma has been described as a diagnostic pitfall cytologicaly by some authors.[8-12] Leni et al. in their study series found only 11 out of 25 cases had a cytohistologic agreement.[12]
It could be mistaken for malignant lesions of the skin, especially squamous cell carcinoma or metastatic carcinoma.[11] In the region of salivary glands, parotid, and submandibular region, it may be mistaken for a mucoepidermoid tumor on cytology because of the presence of squames.[8,9] The aspirate from pilomatrixoma shows anucleate squamous and basaloid cells and not malignant squamous cells, whereas mucoepidermoid carcimona will have predominantly vacuolated cells and malignant squamous cells. The predominance of squamous cells is seen in high-grade mucoepidermoid carcinoma, and squames are unusual. The present case showed squames in abundance. There were no nucleated squamous cells or any vacuolated cells.
When the anucleate squamous cells are seen in clumps, it may resemble the matrix of pleomorphic adenoma; a careful observation will distinguish the two. In pleomorphic adenoma, the matrix is chondromyxoid or fibromyxoid, which will appear as magenta on May-Grünwald-Giemsa (MGG) stain and grayish in Pap stain along with epithelial and myoepithelial cells in groups and clusters.
It is very important to distinguish these lesions in the parotid region on cytology.
Similar to the observation made by some authors, we too found many multinucleated giant cells and macrophages.[3,4]
Another cytological feature observed by few authors is the presence of calcified material, which was not seen on our FNA smears, but was noted in the histopathology sections.[3] The present case did not show pink fibrillary material in MGG smears as noted by Lemos et al. in seven of their nine cases.[4]
|
Conclusion
The FNAC of pilomatrixoma is characteristic and will allow a conclusive diagnosis even in cases with an aberrant clinical presentation
|
References
- Cozzi DA, d’Ambrosio G, Cirigliano E, Negro V, Iacusso C, Totonelli G, et al. Giant pilomatricoma mimicking a malignant parotid mass. J Pediatr Surg 2011;46:1855-8.
- Phyu KK, Bradley PJ. Pilomatrixoma in the parotid region. J Laryngol Otol 2001;115:1026-8.
- Viero RM, Tani E, Skoog L. Fine needle aspiration (FNA) cytology of pilomatrixoma: Report of 14 cases and review of the literature. Cytopathology 1999;10:263-9.
- Lemos MM, Kindblom LG, Meis-Kindblom JM, Ryd W, Willén H. Fine-needle aspiration features of pilomatrixoma. Cancer 2001;93:252-6.
- Dubb M, Michelow P. Fine needle aspiration cytology of pilomatrixoma and differential diagnoses. Acta Cytol 2009;53:683-8.
- Wang J, Cobb CJ, Martin SE, Venegas R, Wu N, Greaves TS. Pilomatrixoma: Clinicopathologic study of 51 cases with emphasis on cytologic features. Diagn Cytopathol 2002;27:167-72.
- Sánchez Sánchez C, Giménez Bascuñana A, Pastor Quirante FA, Montalbán Romero MS, Campos Fernández J, Sola Pérez J, et al. Mimics of pilomatrixomas in fine-needle aspirates. Diagn Cytopathol 1996;14:75-83.
- Sivakumar S. Pilomatrixoma as a diagnostic pitfall in fine needle aspiration cytology: A case report. Acta Cytol 2007;51:583-5.
- Lemos LB, Brauchle RW. Pilomatrixoma: A diagnostic pitfall in fine-needle aspiration biopsies. A review from a small county hospital. Ann Diagn Pathol 2004;8:130-6.
- Wong MP, Yuen ST, Collins RJ. Fine-needle aspiration biopsy of pilomatrixoma: Still a diagnostic trap for the unwary. Diagn Cytopathol 1994;10:365-9.
- Preethi TR, Jayasree K, Abraham EK. A case of pilomatrixoma misdiagnosed as metastatic carcinoma on fine needle aspiration cytology. J Cytol 2007;24:207-8.
- Leni A, Todaro P, Bonanno AM, Catalano F, Catalano A, Tuccari G. Limits of fine-needle aspiration cytology in diagnosing pilomatrixoma: A series of 25 cases with clinicopathologic correlations. Indian J Dermatol 2012;57:152-5.

