

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2019.v05i03.004
Year: -0001, Volume: 5, Issue: 3, Pages: 19-30
Original Article
P Kaushik Ragubathy1, Hemant Adikane2
1Student, Government Medical College, Gondia, Maharashtra, India, 2Department of Community Medicine, Government Medical College, Gondia, Maharashtra, India
Address for correspondence:
P Kaushik Ragubathy, Student, Government Medical College, Gondia, Maharashtra, India. Phone: +91-9168064946. E-mail: [email protected]
Background: Approximately 50 million people worldwide are suffering from dementia, it is the 7th leading cause of death among the elderly. In India, more than 4 million people have some form of dementia 3. According to the World Health Organization, India’s population of those aged over 65, which was 40 million in 1997, is set to increase to 108 million by 2025 and 240 million by 2050.
Aim and Objective: The aim of the study was to study the prevalence of risk factors of dementia among the elderly population residing in a tribal area of Central India.
Materials and Methods: A door to door cross-sectional study was conducted in the rural/tribal area with a pre-designed case record form that investigated the prevalence of risk factors along with measurement of anthropometry and mini-mental state examination was used to categorize subjects according to their mental status.
Results: This study reports high prevalence of risk factors such as hypertension (31.8%), tobacco chewing (25.43%), high waist-hip ratio (24.57%), smoking habit (15.03%), head injury (11%), overweight (9.54%), alcohol intake (9.25%), 71–80 age (9.25%), diabetics (9%), stroke (4.62%), family history of dementia (2.6%), obesity (2.31%), coronary artery disease (CAD) (1.73%), and depression (1.45%).
Conclusions: This study highlights a significant burden of undiagnosed cases of hypertension, diabetes, depression, and CAD all of which are important risk factors for dementia in the community, most of them are poorly controlled. There is a need to identify the large pool of undiagnosed cases of the mentioned morbidities by screening and offer early treatment to avoid complications.
KEY WORDS: Alzheimer’s, dementia, mini mental state examination (MMSE), risk factors, tribal.
Dementia is usually a disease of the elderly and is characterized by progressive loss of memory and other mental faculties such as language, judgment, and planning, impairment of daily activities, and deficiency in social interaction. Dementia impacts personal, family, and societal life.[1] The World Health Organization (WHO) fact sheet suggests, approximately 50 million people worldwide are suffering from dementia; it is the 7th leading cause of death among the elderly.[2] In India, more than 4 million people have some form of dementia. According to the WHO, India’s population of those aged over 65, which was 40 million in 1997, is set to increase to 108 million by 2025 and 240 million by 2050.[3,4] There are no known curative or preventive measures for most types of dementia. Diet and lifestyle could influence risk, and studies suggest that midlife history of disorders that affect the vascular system, such as hypertension, type 2 diabetes, and obesity, increase the risk for dementia including Alzheimer’s disease.[5,6] Treatment for patients with dementia is still mildly effective, usually slowing cognitive decline in the earlier stages without prolonging survival. Thus, the search for modifiable risk factors is an important challenge.[5-7] The disparity in the prevalence rates of dementia and associated disorders between the Western and Indian subcontinent may be accounted for differences in screening techniques, lower prevalence rates of known risk factors (genetic, medical, or environmental) in the Indian subcontinent, and presence of certain novel and unknown protective factors. As there is scarce published information available on geriatric morbidities from a tribal area of central India and considering the magnitude of present problems of dementia and its risk factors which are less explored in the Indian tribal population, this study was conducted with the objective to find the prevalence of its risk factors.[8]
Objectives
The objectives of the study were to study the prevalence of risk factors of dementia among the elderly population residing in a tribal area of central India.
Study setting
The present study was conducted in the rural area of a tribal region in central India which comprises mixed rural and tribal population.
Study population
All the elderly population above 55 years of age residing in the study settings were included in the study.
Study subject
Inclusion criteria
The following criteria were included in the study:
Exclusion criteria
Severely debilitated subjects were excluded from the study.
Study design
For the conduction of the study, a cross-sectional study was conducted.
Study sample size
The sample size was calculated by considering the prevalence of smoking as a risk factor of dementia (33.33%) from study conducted by Tripathi et al. (2012) in Northern India, with 95% of confidence interval (CI) and 5% of allowable error, so sample size of present study comes to 341. A total of 346 subjects have been included in this study.[8]
Sampling procedure/technique
Study subjects were recruited through house to house survey. Face to face verbal interview was conducted using self-designed questionnaire in 346 subjects who fulfilled the inclusion criteria.
Data collection
A pre-designed, semi-structured, and pre-validated case record form was prepared consisting of open- and closed-ended questions. Variables such as age, gender, education, occupation, religion, marital status, current living status, dietary pattern especially oil and salt, alcohol intake, smoking status, family history of dementia, history of head injury, exercise, family environment, and intellectually stimulating activities were included in the study. A clinical examination was carried out of study subjects, including blood pressure measurement with the help of sphygmomanometer by standard guidelines. For screening of dementia, mini- mental status examination scale was used.
Mini-mental status examination
MMSE assesses variable functions such as calculations, attention, recall, language, and orientation. A maximum of 30 points is rewarded on perfectly executing all the given task: For orientation: Ten points, registration: Three points, recall: Three points, attention and calculation: Five points, language: Eight points and copying: One point.
Ethical consideration
Institutional ethical committee permission was taken prior start of the study. All the study subjects having risk factors were counseled and referred to rural health training center for appropriate management of morbidities.
Ethicalclearancereferencenumber:18/2019/20/02/2019
IEC registration number: ECT/1033/INST/MH/2018.
Research question
Are the risk factors of dementia prevalent in rural and tribal societies?
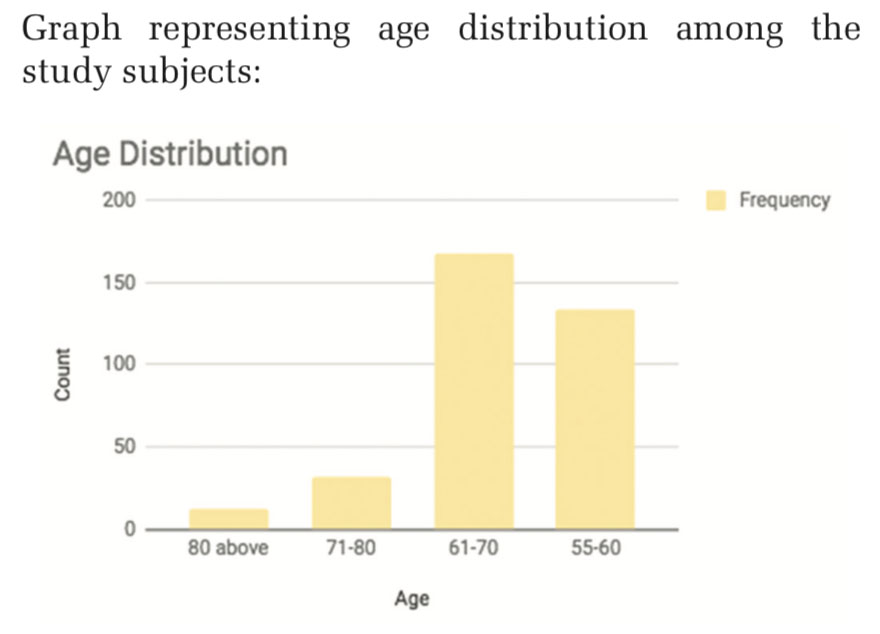
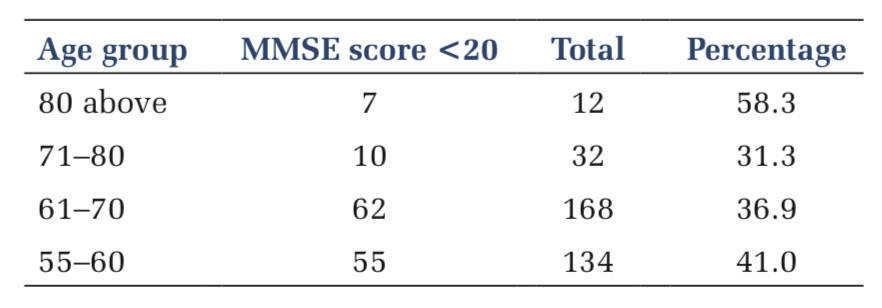
Out of the interviewed 349, 165 were women and 181 men, three subjects were rejected due to their debilitated state, inability to communicate and inability to measure anthropometry. About 38.8% of the study population ranged from 55 to 60, 48.4% being 61–70, and 9.5% being 71–80 whereas only 3.3% being more than 81. Graph representing age distribution among the study subjects:
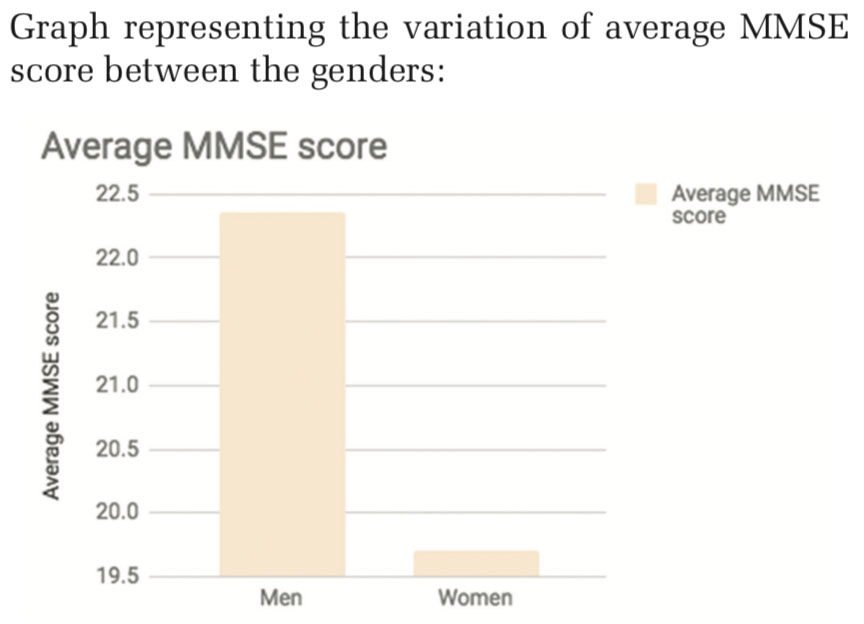
Men consisted of around 52% of the study, the rest 48% of women. Men scored higher average than women.
Graph representing the variation of average MMSE score between the genders:
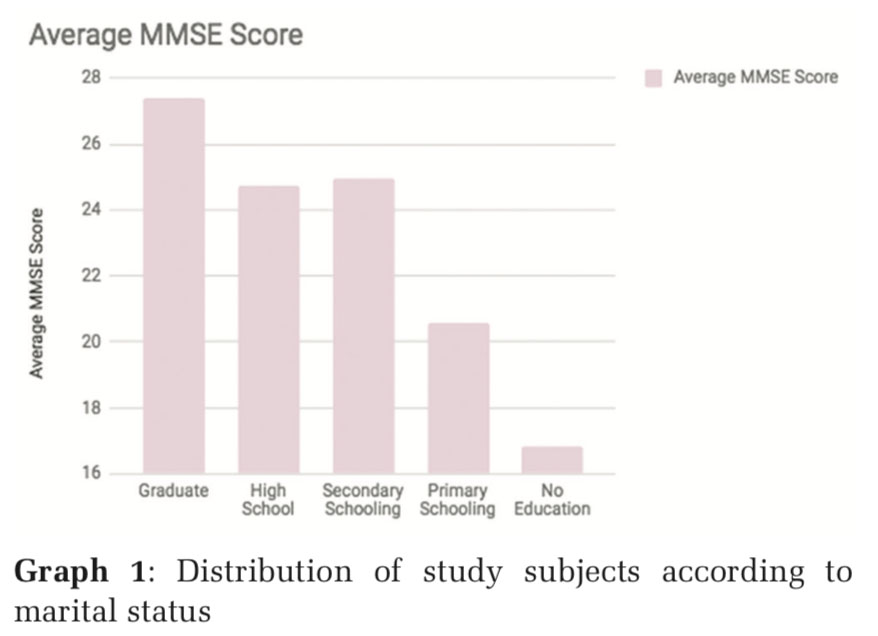
About 38.8% of the study consisted of people with primary schooling (up to 5th grade), 27.7% being uneducated (no schooling at all), 24% up to secondary school, 5.2% up to high school, and 4.3% graduates.
Graph 1 representing MMSE average variation among different level of educational strata:
About 98.5% of the population was married, 0.9% unmarried, and 0.6% widowed.
About 76.3% of the study population belonged to three-generation family, 19.65% to nuclear family, and rest 4.05% to joint families.
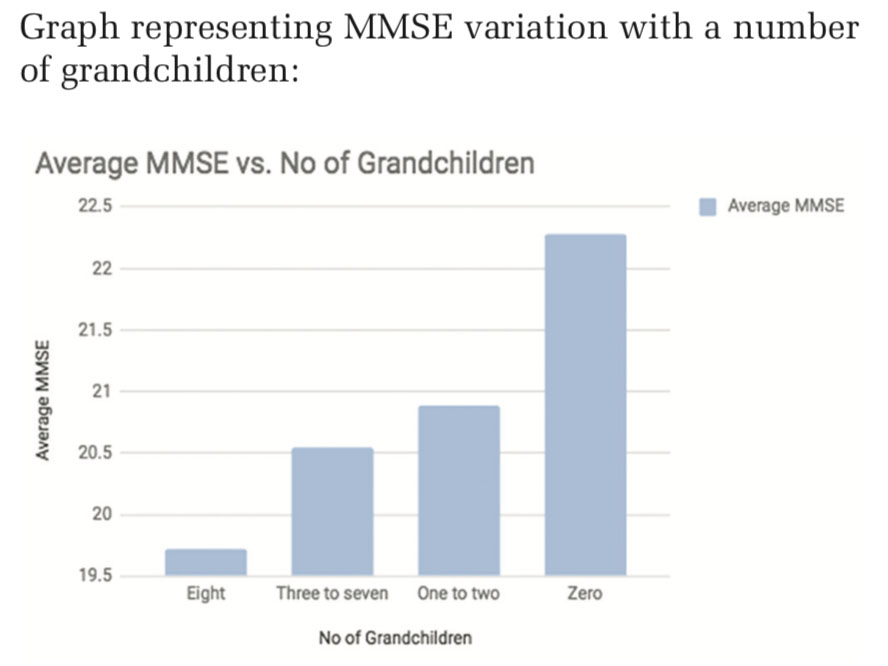
About 23.4% did not have any grandchildren, 39.3% had 1 or 2, 26.9% had 3 or 4, and 10.48 had 5 or more than five grandchildren.
Graph representing MMSE variation with a number of grandchildren:
Only 2.6% of the entire study population had a positive family history for dementia.
About 31.79% had hypertension, 1.73% had coronary artery disease, and 4.62% had a history of stroke.
About 63.58% had a mixed diet, whereas 36.42% were pure vegetarians.
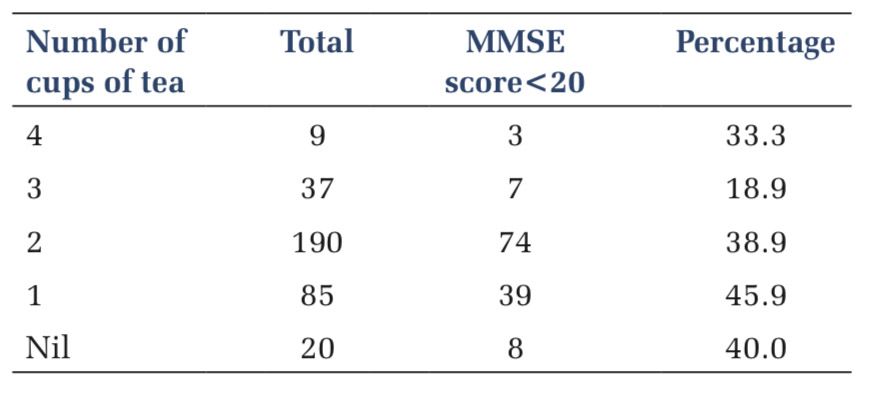
About 10.4% did not consume tea on a daily basis, whereas 20% did consume at least on cup of tea and 69.7% consumed more than one cup.
About 15.03% were smokers and 25.43% were chewed tobacco.
All the subjects (100%) were spiritually inclined.
About 99.71% were actively socializing.
About 3.5% performed strenuous and extreme activity and exercise, 3.5% moderate, and 93% did not exercise at all.
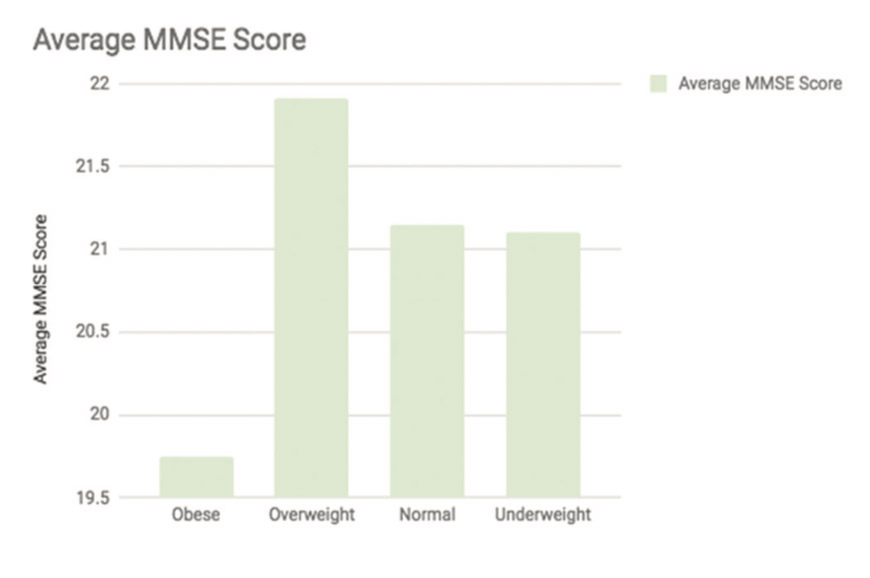
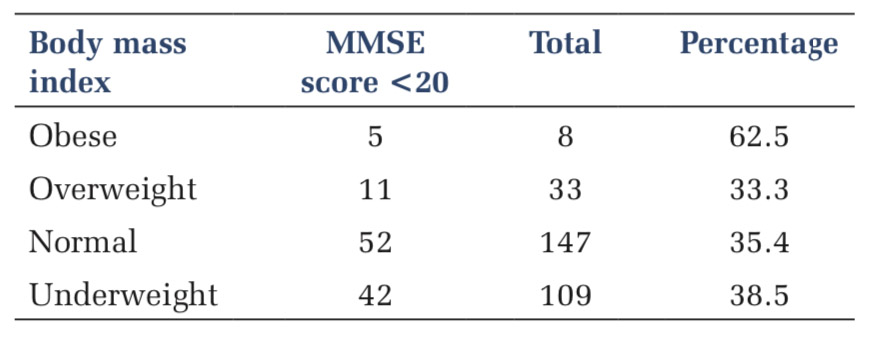
About 43.06% were underweight, 32.66% normal, 19.36% overweight, and 4.91% obese.
Graph representing a variation of MMSE score among different body mass index (BMI) categories:
About 3.76% were undergoing chronic nonsteroidal anti-inflammatory drug (NSAID) treatment.
Around 70% of the total population had one or more than one risk factor.
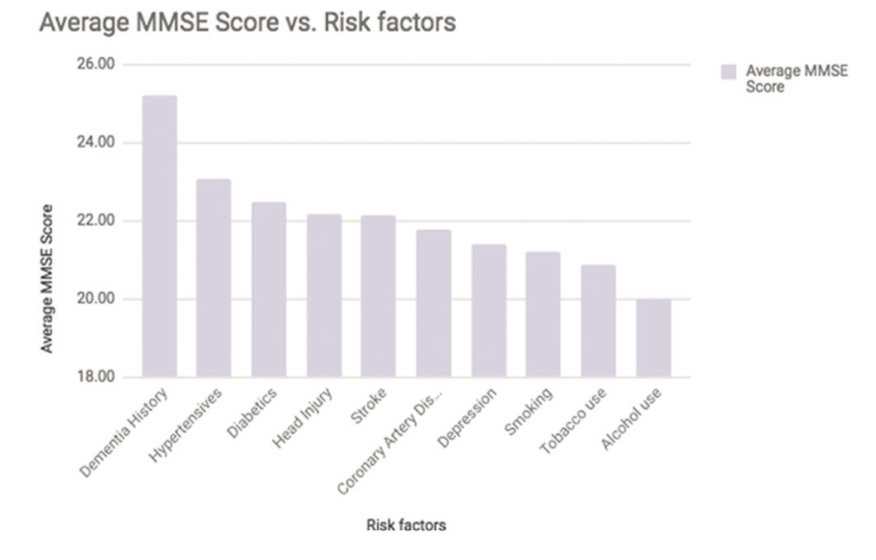
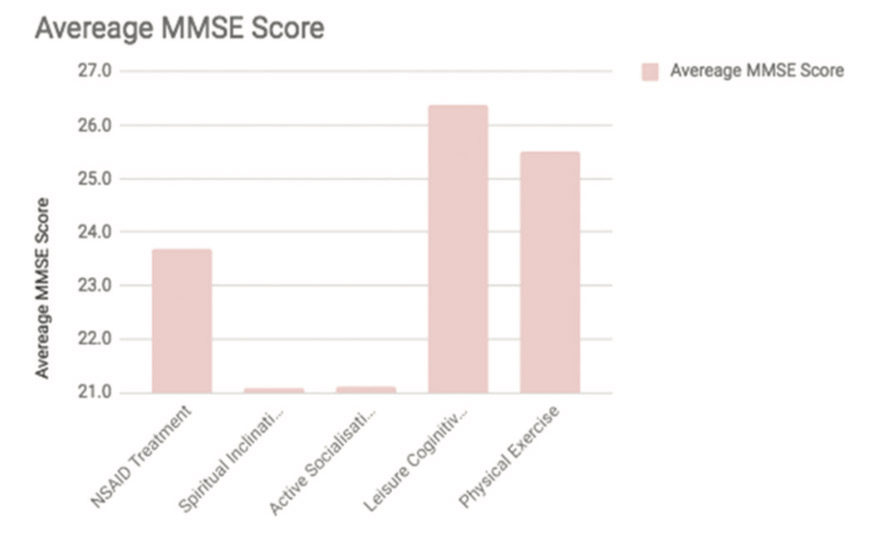
Graph representing MMSE average variation between different risk factors:
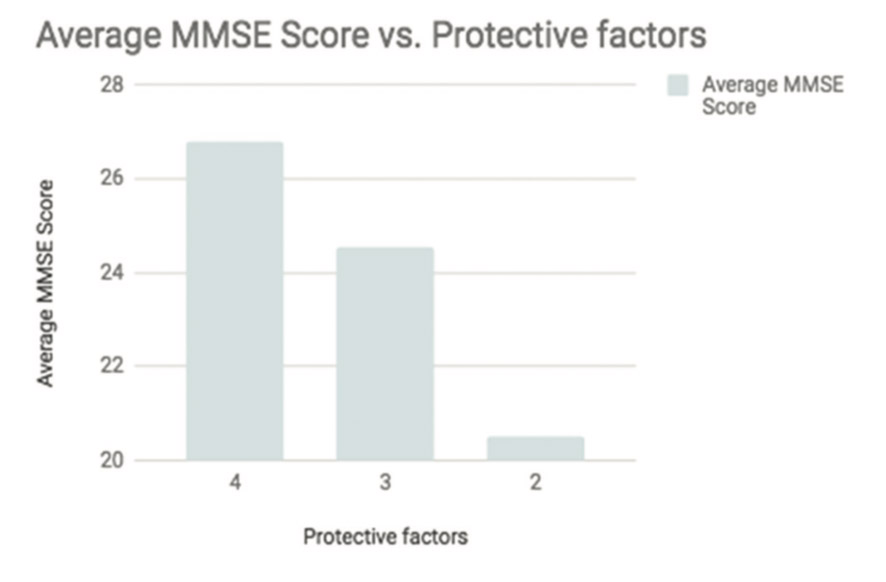
About 11.26% had 3–4 protective factors.
Graph showing MMSE average variations with the number of protective factors:
Graph representing the MMSE average among the protective factors:
Table representing the prevalence of different risk factors:
Out of the 346 study subjects, 242 (70%) subjects have the presence of one or more risk factors present, whereas 104 (30%) of the population have no risk factors present. The positive risk factors consist of a history of dementia in family, diabetes mellitus, hypertension, coronary artery disease (CAD), stroke, depression, smoking habits, tobacco, and alcohol intake and history of head injury.
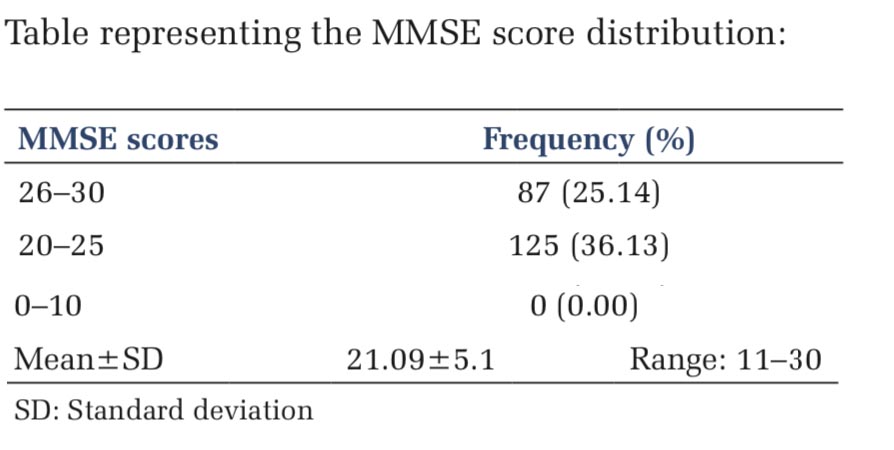
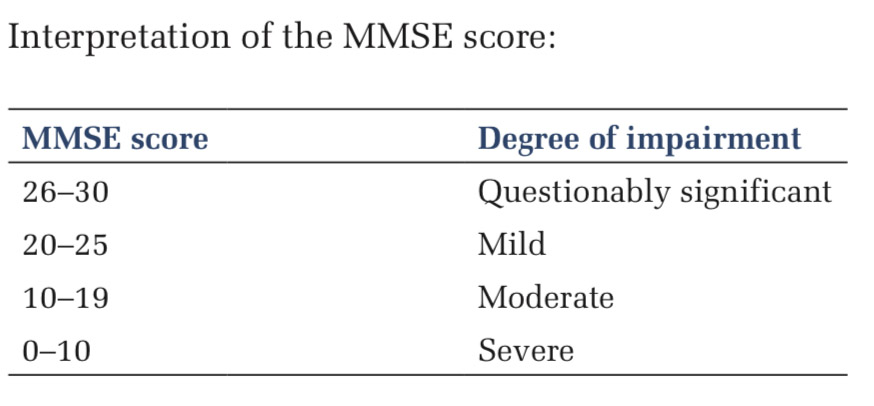
MMSE scoring
Out of the 346 subjects, 87(25.14%) subjects scored 26–30, 125 (36.12%) scored 20–25 whereas 134 (38.72%) scored 10–19.
Mini-mental state examination is a tool developed to evaluate the mental state and concentrates only on the cognitive aspects of mental functions and excludes questions concerning mood, abnormal mental experiences and the form of thinking.[9] Interpretation of the MMSE score:
Age
The mean age of respondents in this study was 63.97 years, lesser than the study of Tripathi et al., which was 65.7, and Chandra et al., which was 66.2. This might be due to (1) lower life expectancy in Indian subcontinent (2) differences in educational, social, economic, and cultural factors including reluctance on the part of the older patients and their families to avail medical services at a modern urban facility due to traditional and religious beliefs, poor transport facilities, and belief in alternative system of medicine in advanced disease in the face of poor response to allopathic medicines. Chandra et al. (1998) reported a prevalence rate of 8.4/1000 in a population aged 55 years and above and an overall prevalence rate of 13.6/1000 in a population aged 65 years and above from a rural community in Northern India.[10]
Several cohort studies have suggested that the risk of dementia and Alzheimer’s dementia (AD) increases with age.[11] A meta-analysis that included 17 Chinese studies has also shown that the prevalence of AD and vascular dementia increases with age.[12] Another population-based longitudinal study shows that the incidence of all-cause dementia is very high in people aged 90 years and older and continues to increase exponentially with age in both men and women.[13]
Gender
The study population consisted of 181(52.3%) males and 165 (47.7%) females. The MMSE scoring average of the males had a higher average as compared to the females. The males had an average of 21.4 whereas females had an average of 19.7. The findings of the previous studies on the impact of gender on dementia suggest that societal factors play an important role in the variation of the disease between both genders. The availability of education, higher education, and jobs to more preferably to males in our society, might play a factor in the higher scoring of the male population in the study. The declining trends of dementia for men and women may vary across countries and across time periods because of the interaction of sex and gender factors with a changing physical, social, and cultural environment (e.g.,interaction of sex and gender with “living conditions”).
The trends for dementia incidence or prevalence may vary by sex. The decline in the incidence of dementia in the Framingham study and in Germany was more pronounced in women than men.[14] Another Dutch follow-up study has found that the incidence of AD in women is higher than that in men after the age of 85 years.[15]
It also reported that the risk of AD declines in men but not in women after the age of 90 years.[16] A meta- analysis that included only Chinese populations has shown a higher prevalence of AD, but not vascular dementia, among women as compared with men aged ≥60 years.
The above findings can be explained by a protective effect of estrogen for premenopausal women and earlier death for men from cardiovascular disease.[12]
On the basis of a systematic literature review conducted on 88 different study population led to a conclusion of the association of dementia and education. A relationship between education and risk for dementia was more consistent in developed compared to developing regions. Age, gender, race/ethnicity, and geographical region moderated the relationship.[17] Another meta-analytic study suggests that a high-level education in early life is related to a significant reduction both in the prevalence and incidence of dementia, including Alzheimer’s disease and vascular dementias.[18]
This prevalence study shows that lower-level education does affect the MMSE scoring which is consistent with other studies.
Risk factors of dementia
About 32 (9.25%) subjects had a history of alcohol abuse of more than 10 years, consuming almost exclusively the “desi” alcohol. Alcohol abuse for more than 10 years is defined as a risk factor. Out of the 32 subjects, 8 (25%) of the subjects had MMSE score of 10–19, signifying a moderate degree of impairment. Heavy alcohol consumption might be associated with an increased risk of dementia in patients with mild cognitive impairment or in men carrying the APOEe4 allele. A J-shaped relationship may exist between alcohol consumption and cognitive decline in mild cognitive impaired patients. Light-moderate alcohol drinking may be associated with decreased risks for dementia in elderly patients with mild cognitive impairment. Heavy drinkers had a higher risk of dementia than abstainers and light-moderate drinkers.[19]
About 52 (15.03%) subjects had a history of smoking for more than 10 years consisting exclusively of locally made “bidis.” Out of the 52 subjects, 9 (17%) of the subjects had MMSE score of 10–19. Smoking was defined as a risk factor if a subject smoked three bidis per day for at least 1 year. A meta-analysis of more than 37 studies was made to assess the correlation between smoking and dementia. It is established that smokers show an increased risk of dementia, and smoking cessation decreases the risk to that of never smokers. The increased risk of AD from smoking is more pronounced in apolipoprotein E ε4 noncarriers.[20]
Five (1.45%) subjects had history of depression, but as of the operational definition, the obtained history of depression is not significant. A history of depression for about 10 years is considered as a risk factor, but the histories obtained have a duration of months to years, which is relatively less significant. None of the subjects scored < 20, and a proper assessment of the relation to the corresponding MMSE score is not possible as the sample size is not adequate. The meta-analytic studies of Gao et al. reported that depression is a major risk factor for the incidence of dementia (including AD, vascular dementia, and any dementia)andmildcognitiveimpairment.[21]
Six (1.73%) subjects had a history of CAD, with a history of heart attack. None of the subjects score < 20, indicating no significant degree of impairment.[8]
Sixteen (4.62%) subjects had a history of stroke with hemiplegia and 7 (43.8%) of the 16 subjects scored < 20.
Thirty-eight (11%) of the subject had a history of head injury. Head injury was defined as positive if it was followed by severe headache, nausea, blurred or double vision, vertigo, amnesia, or loss of consciousness. Twelve (31%) of the 38 subjects scored < 20. According to the retrospective case– control study conducted by Rosso et al., head trauma was associated with a 3.3 times risk for frontotemporal dementia.[22]
Thirty-one (9%) of the subjects had diabetes. Nine (29%) of them scored < 20. Moreover, as found in the study conducted by Cukierman et al., individuals with diabetes had a 1.2–1.5-fold greater change over time in measures of cognitive function than those without diabetes. Type 2 diabetes is associated strongly with insulin resistance, which is related to the formation of Aβ and inflammatory agents in the brain and the subsequent increased risk of AD as stated in the meta-analytic study of Chen et al.
About 110 (31.8%) of the subjects were hypertensives. About 42 (38%) of them scored < 20. According to the finding of Ninomiya et al., midlife hypertension and late-life hypertension are significant risk factors for the late-life onset of vascular dementia.[23] Findings of the meta analytic study of Nagai et al. suggests brain matter damage with cognitive impairment is associated with long standing hypertensive status.[24] Accordingly, strict BP control including during sleep may have a neuroprotective effect on the brain, and thereby prevent the incidence of dementia.
Nine (2.6%) of the subjects had a history of dementia in family, out of which 4 (44.4%) scored < 20. The findings of the prospective study by Wolters et al. suggest that parental history of dementia increases the risk of dementia, primarily when age at parental diagnosis is < 80 years. Furthermore, the findings from Wolters et al. suggest that having a first-degree relative or a parent with dementia was significantly associated with AD risk but having a sibling with dementia was not.[25]
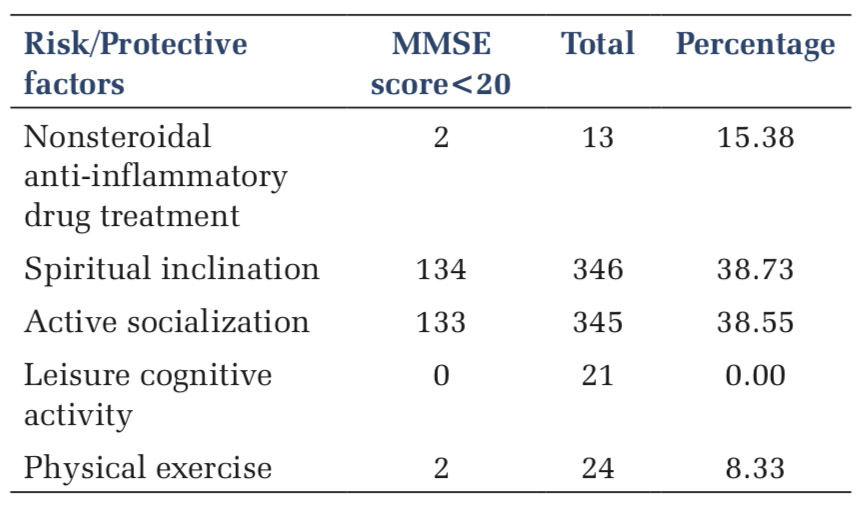
Protective factors
The more the number of protective factors presents the higher is the MMSE average of the individual as observed. The protective factor consists of chronic NSAIDs use, higher cognitively demanding activities, physical exercise, active socialization, and spiritual inclination.
Chronic NSAIDs use was found in 13 (3.75%) of the subjects, of which 2 (15.4%) scored < 20. The cohort studies conducted by Breitner et al. suggested the delayed onset of AD in NSAID users.[26] Another prospective study conducted by Szekely et al. also suggests reduced risk of AD in NSAID users, but this association was found only in those with an APOE ε4 allele, and there was no advantage for Aβ42 lowering NSAIDs.
Twenty-one (6.06%) of the subjects were found to participate in leisure cognitive activities, out of which none scored < 20 in the MMSE. The findings of a prospective cohort conducted by Verghese et al. suggest leisure cognitive activity as a significant protective factor and participation in leisure activities is associated with a reduced risk of dementia. In another study with positron-emission tomography scan imaging between 19 younger and 17 elder individuals conducted by Scarmeas et al., 2003, suggests that the individuals undergoing cognitively stimulating activities clinically tolerate the pathology of dementia by cognitive reserve mediated brain activation.
Twenty-four (7%) of the subjects were found to participate in demanding physical exercises, out of which only two scored < 20. The study of Laurin et al. has indicated that high levels of physical activity were associated with reduced risks of cognitive impairment, Alzheimer disease, and dementia of any type.
About 345 (99.7%) of the subjects were found to be actively social. Acommunity-based cohort study by Fratiglioni et al. provided valuable data on the association of active socialization with dementia. The study indicates that single people or individuals who live alone had an adjusted relative risk of 1.9 (95% CI 1·2–3·1) of developing dementia than those who were married, or living with someone. An extensive social network seems to have a protective effect against dementia. Obesity (BMI, WHR as indicators)
Obesity is defined as an independent risk factor of dementia according to the prospective study conducted by Whitmer et al. Obese people had a 74% increased risk of dementia, while overweight people had a 35% greater risk of dementia compared with those of normal weight. Another prospective study conducted by Gustafson et al. suggest that overweight at high ages is a risk factor for dementia, particularly AD, in women. A higher degree of overweight was observed in women who developed AD at 70–79 compared with nondemented women. For every 1.0 increase in BMI at age 70 years, AD risk increased by 36%.[27]
BMI >25 was found to be an independent risk factor for increased risk of dementia in the study conducted by Tripathi et al.
In this prevalence study, 147 (42.5%) of the study population had a normal BMI (18.6–24.9), 109 (31.5) underweight, 33(9.54) overweight, and 8(2.31) obese subjects.
The MMSE score of the overweight is comparatively higher than the normal BMI subjects. This might be possibly due to the lesser number of overweight subjects, showing a higher average.
About 217 (62.72%) of the subjects had a waist-hip ratio of 0.8–0.89, 29 (8.38%) had WHR of 0.7–0.79, and 85 (24.6%) had WHR of 0.9–0.99. It was found that WHR and BMI were significantly high in the patients of dementia in the study of Tripathi et al. Furthermore, increased BMI and body weight increases the incidences of cardiovascular diseases and diabetes which is again a risk factor for dementia as found in the study of Whitmer et al.
Other factors
According to the study of Tripathi et al., the presence of grandchildren was associated as a risk factor of dementia. In this prevalence study conducted, 265 (76.6%) of the subjects had one or more than one grandchildren.
The association can be due to the fact that people with poor socioeconomic status and low education encourage having a higher number of children and grandchildren as compared to the educated people.[28]
About 126 (36.4%) of the subject was vegetarian whereas 220 (63.6%) of the subject had a mixed diet. All the subjects in the study consumed groundnut oil which is rich in polyunsaturated fatty acid (PUFA).
Dietary factors play a role in the pathogenesis of the disease. An adequate intake of antioxidant micronutrients (e.g., Vitamin C and Vitamin E) and anti-inflammatory macronutrients (e.g.,omega-3 PUFAs) forms an essential component of extrinsic defenses against brain aging. A community-based prospective study on >500 elderly subjects with a Mediterranean diet suggests the high PUFA and monounsaturated fatty acid levels are protective against age-related cognitive decline.[29]
Ten (2.8%) of the subjects had low-calorie intake, 3(0.86%) consumed pickles on a daily basis, and 6 (1.7%) consumed salads on a daily basis. The consumption of pickles was associated with an increased risk of dementia whereas daily consumption of salad was associated with 70% decrease in dementia risk.[8]
In this prevalence study, 9 (2.6%) of the subject consumed around 4 cups, 37 (10.7%) consumed 3 cups, 190(54.9%) consumed 2 cups, and 85 (24.5%) consumed around one cup of tea per day.[8]
Intake of tea more than four cups a day was found to be an independent predictor associated with increased risk of dementia in the study of Tripathi et al.

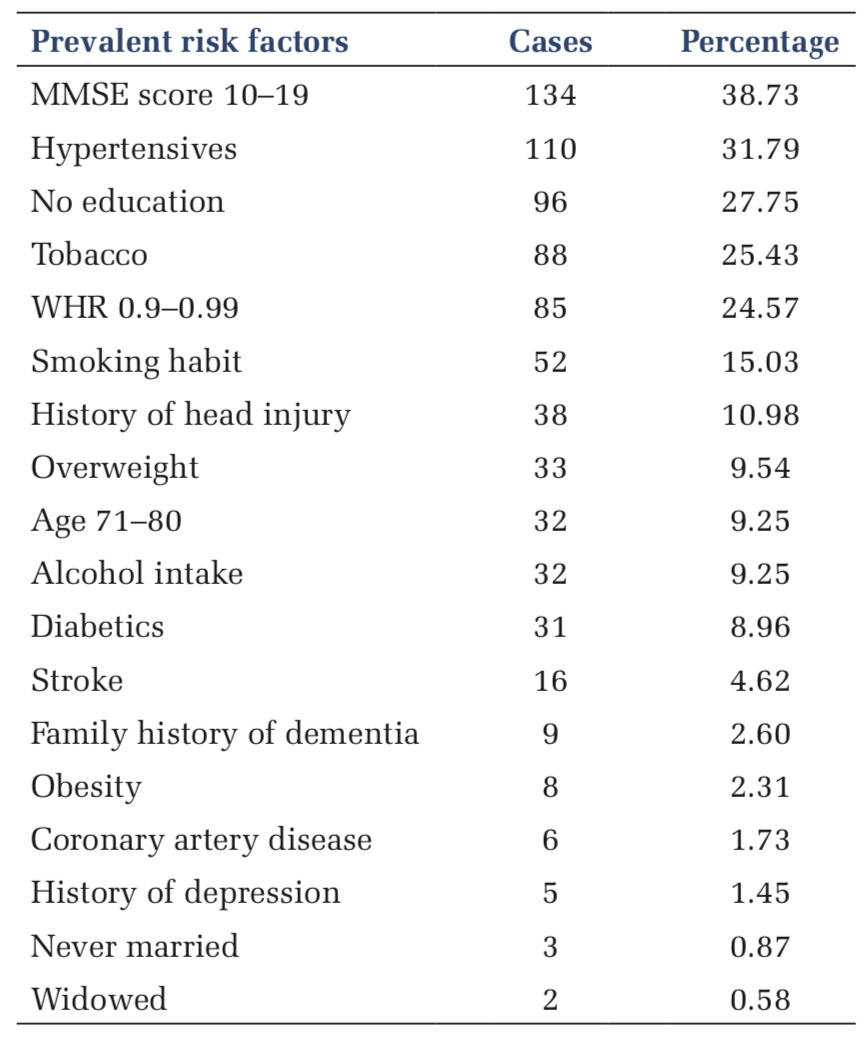
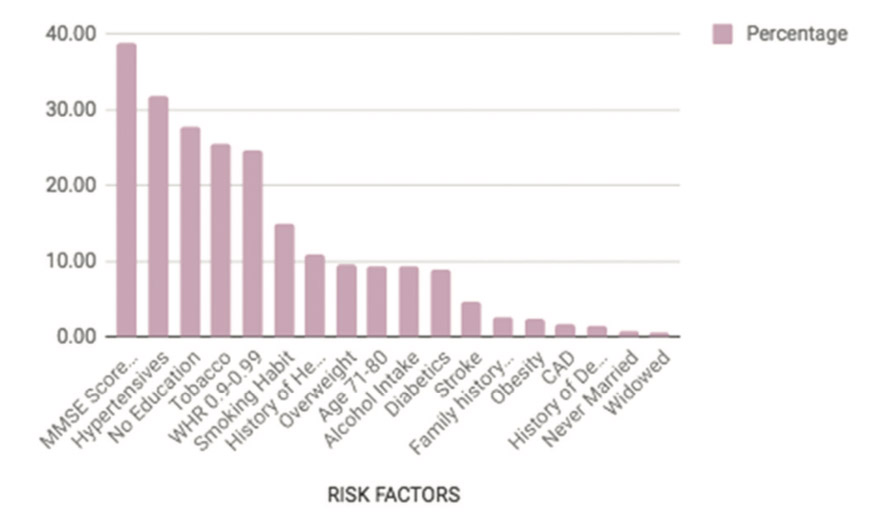
The present study provides reliable and recent epidemiological information regarding the high prevalence of various risk factors of dementia among the elderly population in the rural and tribal population present in Central India. Around 31% of the general adult population suffers from hypertension, which has been found to be the most prevalent. The rest of the morbidities are tobacco chewing (25.43%), high waist-hip ratio (24.57%), smoking habit (15.03%), head injury (11%), overweight (9.54%), alcohol intake (9.25%), 71–80 age (9.25%), diabetics (9%), stroke (4.62%), family history of dementia (2.6%), obesity (2.31%), CAD (1.73%), and depression (1.45%).
This study also highlights a significant burden of undiagnosed cases of hypertension, diabetes, depression, and CAD in the community, which are important risk factors of dementia, most of them are poorly controlled. There is a need to identify the large pool of undiagnosed cases of the mentioned morbidities and offers early treatment to avoid complications since dementia is not curable and can only be controlled. Screening measures should be adapted for early diagnosis and prevention.
Limitations of the study
Since this is a prevalence study of the risk factors, the actual burden of dementia itself on the rural population was not considered. Studies on the prevalence of dementia in rural populations have not been conducted in our country, which would have provided significant data on the risk factors to be studied. Further risk factors such as diabetes, hypertension, depression, and CAD have a chance of being underdiagnosed in the rural population due to the lack of health-care facilities and illiteracy among the rural population. Due to lack of facilities, laboratory testing of significant risk factors such as serum low-density lipoproteins (LDL), high-density lipoproteins, very-LDL cholesterols, triglycerides, homocysteine level, T3, T4, and thyroid-stimulating hormone levels could not be performed.
Subscribe now for latest articles and news.