Introduction
"...when one is called to a case of this kind, it is his duty to look upon his unhappy patient as inevitably doomed to die, unless he can by some active measure wrest her from the grave already yawning before her. "— John Parry, 1876.
The blastocyst usually implants in the endometrial lining of the uterine cavity following fertilization and 1 and comprises 3-4 per cent worldwide incidence. The incidence of ectopic pregnancy has risen in the past 20 years due to various predisposing factors and also better diagnostic techniques. The aetiology of ectopic pregnancy remains undetermined though several risk factors have been related 2. This condition disparately accounts for 6 percent of all pregnancy-related deaths3 and also lessen the possibility of a subsequent successful pregnancy. Fortunately, urine and serum beta-human chorionic gonadotropin (β-hCG) assays and transvaginal sonography have made earlier diagnosis feasible4 and thereby both maternal survival rates and conservation of reproductive capacity are improved. Ectopic pregnancy is one of the few obstetric ailments that can be treated expectantly, medically or surgically 1, 5.
Nearly 95 percent of ectopic pregnancies are implanted in the various segments of the fallopian tube and give rise to fimbrial, ampullary, isthmic, or interstitial tubal pregnancies. The ampulla is the most frequent site, followed by the isthmus. The remaining 5 percent of non-tubal ectopic pregnancies implant in the ovary, peritoneal cavity, cervix, or prior caesarean scar. Occasionally, a multifetal or heterotopic pregnancy occurs with one conceptus with normal uterine implantation coexisting with another implanted ectopically.
Infertility, per se, as well as the use of ART to overcome it, is linked to substantively increased risks for ectopic pregnancy 6. Artificial reproductive technologies (ART), has increased their incidence to 1 in 7000 overall, and following ovulation induction, it may be as high as 0.5 to 1 percent7 Smoking is also a known association, although the underlying mechanism is unclear 8. Abnormal fallopian tube anatomy underlies many cases of tubal ectopic pregnancy. Surgeries for a prior tubal pregnancy for fertility restoration, or sterilization confer the highest risk of tubal implantation. Prior sexually transmitted disease or other tubal infection, which can distort normal tubal anatomy, is another common risk factor. Similarly, peritubal adhesions subsequent to salpingitis, appendicitis, or endometriosis may increase the risk for tubal pregnancy. Chlamydia trachomatis has been associated with 30-50% of all ectopic cases 9. The threat of ectopic pregnancy multiplies with increasing maternal age, with age more than 35 years being a substantial risk factor 5. Women with a preceding history of ectopic pregnancy also have an elevated risk, in proportion to the number of previous ectopic pregnancies. In one observation, the OR for having another ectopic pregnancy was 12.5 after previous single episode and 76.6 after two such 10. Lastly, with any form of contraception, the absolute number of ectopic pregnancies has diminished but the failure of some contraceptive methods like tubal sterilization, copper and progestin-releasing intrauterine devices (IUDs)11 has led to the rise of the relative number of ectopic pregnancies.
The usual presentation of ectopic pregnancies are pain and vaginal bleeding between 6 and 10 weeks gestation 1. However, these are frequent and non-specific features in early pregnancy, experienced by almost one third of the mothers 12. The pain can be continuous, relentless and is frequently unilateral. Shoulder-tip pain, syncope and shock are the manifestations of about 20% women and abdominal tenderness in greater than 75%. Cervical motion tenderness has been elicited in almost 67%, and a palpable adnexal mass in 50% approximately 12. Contemporary reports reveal that one third of mothers with ectopic pregnancy present no clinical signs and 9% are asymptomatic 13. Unfortunately, atypical presentation is not rare. This grave disorder may mimic other gynaecological, gastrointestinal or urinary tract diseases, including salpingitis, ruptured corpus luteum or follicular cysts, threatened or inevitable abortion, ovarian torsion appendicitis, urinary tract infection etc. The inquiries and reviews of maternal deaths emphasized that most maternal demises from ectopic pregnancy were initially misdiagnosed in the primary or emergency health-care settings 13.
Materials and Methods
This was an observational cross-sectional study from 1.4.2015 to 31.3.2016 incorporating 100 ectopic pregnancies in the ANC clinic or admitted in the Maternity ward of the Department of Obstetrics & Gynaecology, BSMCH, Bankura, West Bengal, India after informed consent. The inclusion criteria were female of child-bearing age group complaining of pain in lower abdomen, bleeding per vagina with history of amenorrhoea for certain period, in whom urine pregnancy test for β−HCG was positive and clinically or sonologically confirmed to be a case of ectopic pregnancy. Patients refusing for study participation or patients in gasping condition or expired prior to interview were excluded. Detailed history of each patient compiling patient particulars, chief complaints with onset and duration, menstrual and obstetric history including history of subfertility, previous tubal surgery, history of abortion which needed dilatation and curettage, choice of contraception like IUD, contraceptive pill or permanent methods were recorded. The socio-economic status was assessed by Modified Kuppuswamy scale. Clinical evaluation included general examination like presence of pallor, features of shock, abdominal examination for signs of haemoperitoneum, guarding, rigidity, tenderness. Abdominal paracentesis was also helpful in diagnosis of haemoperitoneum. Examination per vagina was done to estimate the size of uterus, bleeding, cervical motion tenderness etc. USG was done in almost all suspected cases. All 100 cases were managed surgically through laparotomy where Salpingectomy, Salpingostomy were the procedures done to tackle the situation. Patients were followed up post-operatively till complete recovery. Diagnosis was confirmed by histopathological examination.
Statistics
For statistical analysis data were entered into a Microsoft excel spreadsheet and then analysed by SPSS (version 27.0; SPSS Inc., Chicago, IL, USA) and Graph-Pad Prism version 5. Data was summarized as mean and standard deviation for numerical variables and count and percentages for categorical variables. Data was analysed thereafter.
Results
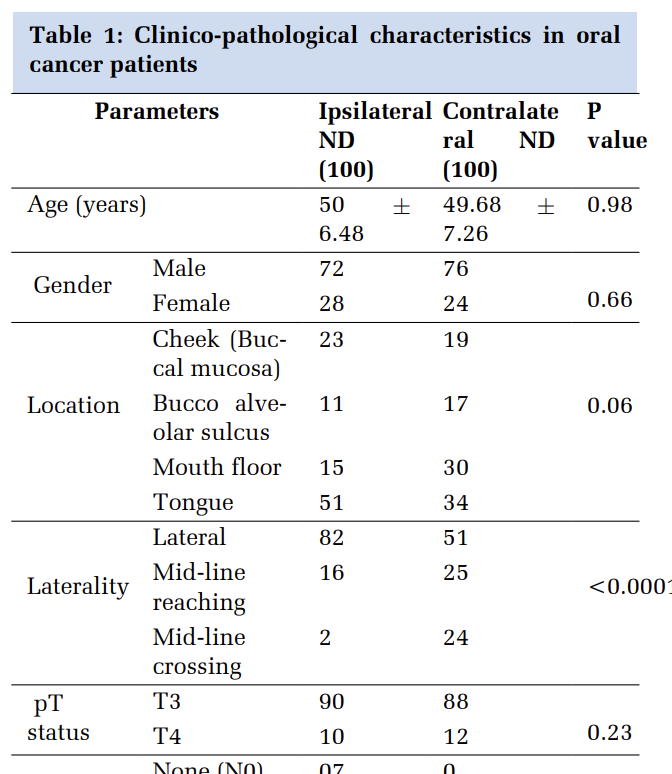
In our study the highest number of cases (38%) were in the age group of 26-30 years followed by 30% in 21-15 years. 18% were primigravida and the rest multigravida. 80% of the ectopic pregnancies under consideration belonged to low socio-economic group, 12% to middle and a few i.e. 8% from high strata as per Modified Kuppuswamy scale [Table 1].
The risk factors taken into consideration were history of PID (23%), history of dilatation and curettage (20%), previous tubal surgery (21%), use of oral contraceptive pills (5%), use of Cu-T (1%), previous ectopic (1%), history of subfertility and ovulation induction (6%) [Table 2].
|
Criteria |
Classification |
Number of Cases |
|
Age |
≤ 20 years |
13 (13%) |
|
21-25 years |
30 (30%) |
|
|
26- 30 years |
38 (38%) |
|
|
30-35 years |
15 (15%) |
|
|
>35 years |
4 (4%) |
|
|
Gravida |
Primigravida |
18 (18%) |
|
2nd gravida |
34 (34%) |
|
|
3rd gravida |
35 (35%) |
|
|
>3rd gravida |
13 (13%) |
|
|
Socio-Economic Status |
Upper |
8 (8%) |
|
Upper Middle |
4 (4%) |
|
|
Lower Middle |
8 (8%) |
|
|
Upper Lower |
36 (36%) |
|
|
Lower |
44 (44%) |
|
Risk Factor |
Number of Cases |
|
History of PID |
23(23%) |
|
Previous Dilatation and Curettage |
20 (20%) |
|
Previous tubal surgery |
21 (21%) |
|
OCP use |
5 (5%) |
|
Use of Cu-T |
1 (1%) |
|
Previous ectopic |
1 (1%) |
|
History of subfertility and ovulation induction |
6 (6%) |
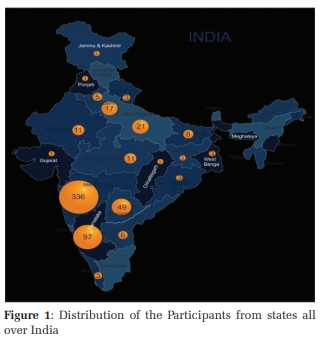
98% of patients presented with complaints of pain abdomen establishing it as the most consistent symptom of ectopic pregnancy 90% of the patients had a history of amenorrhoea of variable period extending upto 5 months and 82% had bleeding per vagina [Figure 1].

Table 3 shows 97% of patients presented with pallor. Shock was defined as pulse >100 bpm & BP <90/60 mmHg. 23 patients presented with shock at the time of admission and cervical motion tenderness could be elicited in 73 %. Abdominal paracentesis was done in 46 cases of which 27 yielded frank blood on aspiration (positive).
|
Sign |
Occurrence |
Number of Cases |
|
Pallor |
Present |
97 (97%) |
|
Absent |
3 (3%) |
|
|
Shock |
Present |
23 (23%) |
|
Absent |
77 (77%) |
|
|
Cervical Motion Tenderness |
Present |
73 (73%) |
|
Absent |
27 (27%) |
|
|
Abdominal Paracentesis |
Positive |
27 (27%) |
|
Negative |
19 (19%) |
|
|
Not done |
54 (54%) |
Urine for pregnancy test was positive in all cases and USG was possible for 98 patients. Sonography revealed an adnexal mass in 95 and free fluid in POD in 92 patients [Figure 2]. 100% of cases were managed surgically and taken for laparotomy. On opening the abdomen, ruptured ectopic was noted in 64% and haemoperitoneum in 67 % of the cases [Figure 3]. 47% of ectopic pregnancies were left sided and the rest in the opposite end and ampulla was the commonest site of involvement (76%) [Figure 4].



Discussion
The incidence of ectopic pregnancy is approximately 1.5-2% of all pregnancies. The incidence increased dramatically, by about 6-fold, between 1970 and 1992 but the risk of death related to ectopic pregnancy decreased by almost 90% 14. In our study we found the incidence was about 0.45%. An analysis of 114 cases by Samiya Mufti et al15 showed incidence was highest in 26 to 30 years of age group (55.25%). Our study also deduced the highest incidence in this age group (38%). They also observed that highest incidence in primigravida (53.5%) whereas the highest incidence according to our data was in 3rd and 2nd gravida i.e. 35% and 34% respectively. Older age and low socio-economic status were associated with ectopic pregnancy as per Yuk JS et al16 similar to our findings where 80% cases belonged to low socio-economic strata.
Barnhart and colleagues reported a strong association between prior PID and ectopic pregnancy with OR ranging from 2.0 to 10.1 17 while in our analysis 23% patients of ectopic pregnancies had previous history of PID. It has been observed that previous tubal surgery is a major predisposing factor for abnormal implantation with an estimated OR of 4.7 (2.4-9.5) according to a meta-analysis. 18 Among contraceptive methods, use of intrauterine device was significantly related to ectopic compared with the women without any birth-control method 19. The chances of ectopic was almost 17 times higher for women who had prior similar episode in comparison with controls (OR = 17.165, 95% CI = 1.89–155.67) 19. Barnhart et al.17 emphasized that the risk of facing another ectopic elevates intensely with the number of previous ectopic pregnancies (OR = 2.98 for one prior EP and OR = 16.04 for 2 or more). History of subfertility, especially primary infertility was another factor linked to ectopic with an OR of 6.135 (P < 0.0001) 19. In our observation the other predisposing agents were previous tubal surgery (21%) history of Dilatation and curettage (20%), pre-existing subfertility and ovulation induction (6%), previous OCP (5%) and Cu-T (1%) usage and history of ectopic (1%) respectively.
Only about 50% of patients as per our analysis presented with the classical triad of symptoms. In one case series of ectopic pregnancies, abdominal pain presented in 98.6% of patients, amenorrhea in 74.1% of them, and irregular vaginal bleeding in 56.4% of patients 20. In our study it was noted that history of amenorrhoea was present in 90% of cases, pain abdomen in 98% and bleeding per vagina in 82% which were almost similar with the previous study. 9.4% were admitted with features of shock in a survey done with 180 cases of ectopic pregnancy by Majhi AK et al. 21. In our observation, 23% patients were admitted with shock which was more than double of that in the aforesaid study. We had 73% patients with cervical motion tenderness which is almost similar with the study of Majhi AK (82.2%) 21. Abdominal paracentesis was done in 46 cases out of 100 of which 27 cases yielded frank blood on aspiration (positive). Majhi AK et al.21 in their study showed that culdocentesis supported diagnosis in 73.3% cases out of 135 patients. But in our study culdocentesis was not done and was a limitation.
As per the USG findings (done in 98 cases), we found 95% patients with adnexal mass, 3% without adnexal mass and empty uterine cavity and in 92% free fluid in POD. According to Condous G et al., overall, approximately 60 percent of ectopic pregnancies are seen as an inhomogeneous mass adjacent to the ovary; 20 percent appear as a hyperechoic ring; and 13 percent have an obvious gestational sac with a fetal pole 22.
After laparotomy we discovered 64% ruptured ectopic, 33% unruptured and only 3 cases of tubal abortion with hemoperitoneum in 67%. Majhi and colleagues 21 found 70.2% ruptured, 19.9% tubal abortion and 9.9% unruptured cases in their research.
Gandhari Basu et al. 23 had done a cross-sectional study in a sub urban teaching hospital of West Bengal on “Epidemiology of ectopic pregnancy”. They found right side of the tube was affected in 59.2% patients. We found 53% in right side which matches with the aforesaid analysis.
Bouyer24 in the 10-year population-based study in 1800 ectopic pregnancies shown different sites of implantation as follows: in abdominal cavity (1%), in ovary (3%), in fallopian tubes (95%), in cervix (<1%) and in very minor number of cases in broad ligament and rudimentary horn of uterus. In our study we found 95% in fallopian tubes, 5% in ovary without any case of cervical ectopic. Overall incidences of ampullary, isthmic, fimbrial and interstitial implantation were 70%, 12%, 11% and 2-3% respectively24 which nearly corroborated with our survey.
There were certain limitations in our study.
-
This was an observational study and not a randomized control trial.
-
Follow up not done in this study.
-
Culdocentesis is an important aid to diagnose ectopic pregnancy which could not be done in this observation.
-
No patient in our study was benefited by medical or expectant management as all were managed surgically.
-
Laparoscopy though gold standard treatment option nowadays, could not be availed.
Novelty of the Study
Ectopic pregnancy is a potentially lethal situation and is still considered to be one of the prime causes of maternal death, especially in developing countries. The incidence is relatively static or shows an increasing trend and thus, is a matter of emphasis even in the present-day world. This study elaborates the background, clinical features and management and the results or outcome, thereby, provide an overview of this dreaded condition in a limited resource, semi-urban institution and may benefit and guide the health-care workers in similar settings.
Conclusion
Hence, for any patient of reproductive age group presenting with pain abdomen or menstrual irregularity, we should be ectopic-minded. Awareness is needed from the part of doctors, health professionals and patients in order to avert the grave complications of this dreaded condition.
Ethics
The study was approved by the Ethical Review Committee of Bankura Sammilani Medical college and Hospital, Bankura, West Bengal, India. Written informed consent was obtained from each participant or from parents or legal guardians of minors prior to study inclusion.
Conflicts of Interest
The authors declare that they had no competing interests.
Funding
Not applicable.
Author Contributions
All the authors were involved in study concept and design. AT executed data collection, analysis and interpretation under guidance of DS. JM, GB, MM, AT drafted the manuscript. SKB, DS helped in revising it critically. All the authors read and approved the final manuscript.
Acknowledgment
We would like to thank everyone who has made this study possible including those mothers who willingly participated inspite of their physical agony. We convey our gratitude to Prof (Dr.) Subhendu Dasgupta, Head of the Dept., G & O, Prof. (Dr.) G. Basu, Prof. (Dr.) A.K. Das, Dr. B. Chakraborty (Associate Professor), Dr. A. Mondal (Associate Professor), and all the faculties of the Department of Obstetrics and Gynaecology, B.S. M.C.H., and C.O.M.J.NM.H, for their rich support, guidance, constant encouragement and recent updates in the field.
Abbreviations
PID— Pelvic Inflammatory Disease; β-HCG— Beta Human Chorionic Gonadotropin; UPT— Urine Pregnancy Test; ART– Artificial Reproductive Techniques; BSMCH— Bankura Sammilani Medical College and Hospital; Cu-T– Copper-T; OCP— Oral Contraceptive Pill; OR— Odds Ratio; USG— Ultrasonography; POD— Pouch of Douglas