

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.v11.i3.25.138
Year: 2025, Volume: 11, Issue: 3, Pages: 258-262
Original Article
Anoop Sharma1 , S Santhosh Kumar2 , Vidhu Bhatnagar3 , Nikhil Kumar Mestha4 , P Swapna4 , Saurabh Tandon4
1Assistant Professor, Department of Anaesthesia, INM INHS Asvini, Mumbai, Maharashtra, India,
2Senior Resident, INM INHS Asvini, Mumbai, Maharashtra, India,
3Professor, INM INHS Asvini, Mumbai, Maharashtra, India,
4Assistant Professor, INM INHS Asvini, Mumbai, Maharashtra, India
Address for correspondence: Anoop Sharma, Assistant Professor, Department of Anaesthesia, INM INHS Asvini, Mumbai, Maharashtra, India.
E-mail: [email protected]
Received Date:17 April 2025, Accepted Date:07 June 2025, Published Date:20 October 2025
Background: Laparoscopic surgery is popular alternative to open surgery. Laparoscopic surgeries use carbon dioxide to improve visibility and create operating space for instrumentation. But this can increase intracranial pressure (ICP). This study aims to evaluate the effect of propofol and dexmedetomidine on ICP during laparoscopic surgeries by measuring the optic nerve sheath diameter (ONSD), an alternative measure for ICP.
Methodology: A randomized, double-blind clinical trial was conducted with 60 adult patients scheduled for elective laparoscopic surgery. Patients were randomly allocated to either propofol or dexmedetomidine group. Thirty patients received dexmedetomidine infusion at a rate of 0.5 mcg/kg/h, while the other 30 patients received a propofol infusion at a rate of 100mcg/kg/min during balanced anaesthesia after pneumoperitoneum was established. Baseline monitoring was carried out to ensure stable physiological conditions. ONSD measurements in both eyes were taken post-induction and pre-pneumoperitoneum establishment (basal value). Subsequent ONSD measurements were taken during the first 0–15-minute interval after pneumoperitoneum establishment, the second 15–30-minute interval, and the final ONSD measurement after release of pneumoperitoneum.
Results: Demographic characteristics and baseline ICP levels were comparable in both the groups. The dexmedetomidine group showed notably reduced intraoperative ICP values in comparison to the propofol group during laparoscopic surgery (p < 0.05).
Conclusion: To conclude, patients undergoing laparoscopic surgery, dexmedetomidine was found to be better in decreasing ICP compared to propofol.
Keywords
Intracranial Pressure, Optic Nerve, Ultrasonography, Pneumoperitoneum
Laparoscopic surgery is common alternative for open surgery. Laparoscopic surgeries are minimally invasive. Laparoscopic procedures offer better cosmesis, associated with lower postoperative pain scores, enhanced recovery and hence, reduced length of stay at hospital. 1 The pneumoperitoneum for abdominal laparoscopy is created using carbon dioxide (CO2). Pneumoperitoneum increases intra-abdominal pressure. The elevated intra-abdominal pressure results in an elevated intracranial pressure (ICP). 2, 3 Multiple physiological changes are associated with pneumoperitoneum: elevated airway pressure, reduced lung compliance, increased mismatch in ventilation/perfusion, decreased venous return, elevated systemic vascular resistance, hypercapnia and respiratory acidosis. 4, 5
Gold standard technique to measure the ICP is external ventricular drain (EVD) placement. Although being the most accurate method for measuring ICP, it is invasive and can cause neurological injury, intracranial haemorrhage, and infection. 6 The use of these high-risk invasive procedures to measure ICP during routine laparoscopic surgery is not needed. Compared to EVD, the ultrasound measurement of ONSD offers a simpler, non-invasive, and convenient method for bedside ICP monitoring. It allows for the observation of changes in ICP at any point during the surgery. 7 Anaesthetic agents have variable effects on ICP. Volatile anaesthetic agents are potent cerebral vasodilators and alter the ICP in a dose-dependent manner. 5 Dexmedetomidine is highly specific and potent alpha-2 adrenergic receptor agonist. Dexmedetomidine stimulates postsynaptic alpha-2 adrenergic receptors on the cerebral blood vessels that causes cerebral vasoconstriction and decreased cerebral blood flow. 4, 5 Propofol is a gamma-aminobutyric acid agonist. Propofol exhibits a dose-dependent effect on the contraction of cerebral blood vessels, as well as the inhibition of cerebral metabolic oxygen rate and reduction of ICP.
Hansen et al, in their research, discovered a robust association between intracranial pressure and ONSD. Maissan et al, suggested that the optic nerve sheath diameter (ONSD) could potentially serve as a real-time indicator of ICP. After a review of the relevant literature, the authors found contradictory findings, highlighting the need for additional research. This work may provide additional evidence to understand the changes in ICP during laparoscopic procedures. 5, 6, 8, 9, 7, 10
Therefore, we aimed to evaluate the impact of dexmedetomidine and propofol on potential alterations in intracranial pressure by monitoring ONSD in patients undergoing laparoscopic surgery, which is a valuable non-invasive technique for evaluating intracranial pressure.
This was a prospective double-blind randomized controlled study. Approval from the institutional ethical committee (IEC No. 03 dated 12 Sep 2022) was taken. The study was registered with CTRI (clinicaltrials.gov) with registration number CTRI/2022/10/046896. The study was conducted at a tertiary care hospital in Mumbai, between September 2022 to December 2023. While conducting the research all guidelines as per declaration of Helsinki and good clinical practice were followed.
Sample size was calculated with the formula [n=Z2-p(1-p)/E2], with a confidence interval of 95%, estimated prevalence of 4% and margin of error 5%. Sample size calculated was 60. Simple randomization technique was used to make two group of patients: propofol group and dexmedetomidine group. Thirty patients were allocated in each group. Concealment of allocation to either group was ensured by serially numbered opaque sealed envelope technique. Patient and observer were blinded about the drug being used for the study. All adult patients between 18 to 65 years of age, American Society of Anesthesiologists (ASA) physical status I and II, undergoing laparoscopic surgery and consented for participation were enrolled in the study. Patients with neurological, endocrine and psychiatric disorders, patients with pre-existing ophthalmic diseases and ocular injuries, ASA physical status III and above, patients with known allergies to drugs used in the study were excluded.
Written and informed consent was taken from the participants. Patients who met the criteria were included in the study. In operation theatre monitors were attached and baseline readings of heart rate, non-invasive blood pressure (NIBP), respiratory rate, pulse oximetry (SpO2), and electrocardiography (ECG) tracings were recorded. Preoxygenation with 100% oxygen was done. The patients were premedicated with injection fentanyl (2mcg/kg) intravenously (iv). Patients were induced with propofol (2mg/kg) iv and intubated with non-depolarising muscle relaxants (vecuronium-0.1mg/kg). Intraoperative monitoring: ECG, NIBP, SpO2, pulse rate, respiratory rate, end-tidal CO2 (ETCO2) and anaesthesia gas monitor (AGM) for minimum alveolar concentration (MAC) were recorded. Depth of anaesthesia was maintained using 50% O2 + 50% air, nondepolarizing muscle relaxants (vecuronium) and inhalational agents (sevoflurane). ETCO2 was maintained within the range of 30–40 mmHg by adjusting the ventilatory settings. ONSD was measured by observer who was blind for the drug used, after intubation but before pneumoperitoneum and labelled as ‘A’ (Basal value). ONSD was again measured after pneumoperitoneum and labelled as ‘B’. The drug used in the study was prepared as an infusion in 50 ml syringes. Rate of infusion of Dexmedetomidine was 0.5 mcg/kg/h and propofol was 100 mcg/kg/min for 15 to 30 min. During this phase the target MAC was 0.6-0.9. Fifteen to thirty minutes later, when all the physiological changes related to pneumoperitoneum are plateaued, third reading of ONSD was taken by the observer and labelled as ‘C’. Fourth reading of ONSD was taken after desufflation of pneumoperitoneum and labelled as ‘D’. The difference between ‘B’ and ‘C’ reading was calculated. ONSD readings ‘A’ and ‘D’ were taken to confirm whether the ICP reaches to normal values after desufflation.
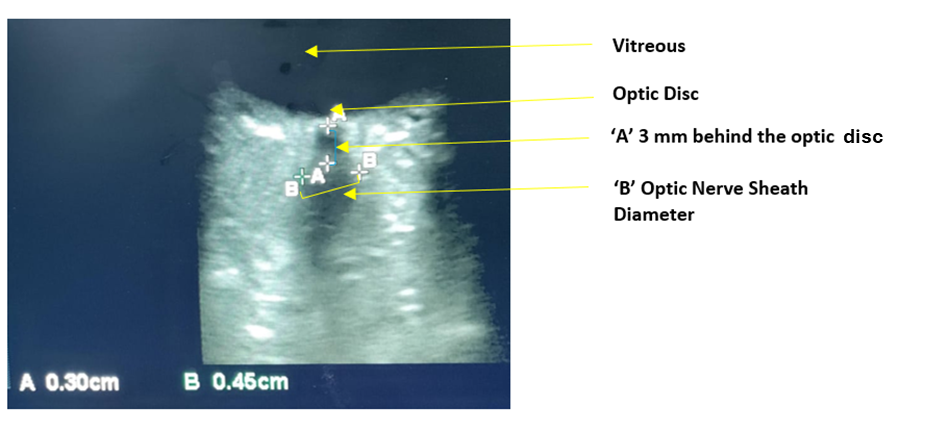
The measurement of ONSD is done using an ultrasound machine. High-frequency linear probe (6-15MHz) is used. The patient is positioned supine with the head in a neutral position and eyes closed. A disposable clear patch is placed over the eyes. A water-soluble ultrasonic gel is spread on the probe and delicately positioned on the upper eyelids without applying any force on the eyeball. A hypoechoic area in the shape of a "long strip" can be observed, positioned perpendicular to the eyeball [Figure 1]. The high echo sheath structure is visible at the border of the hypoechoic area. ONSD is the measurement of the distance between these high echo sheath structures. The ONSD was measured in the transverse plane, 3mm behind the optic disc, using electronic callipers in both the eyes [Figure 1]. Normal values of ONSD are less than 5 mm.
Utilizing the statistical software IBM SPSS version 22, the collected data was entered and analysed in Libre Excel. Percentages were used to report categorical variables, whereas mean and standard deviation were used for continuous variables. The analysis of the means between the two groups was conducted using the student t-test. Significance was determined by a p-value of less than 0.05.
The study included a total of 60 patients, with 30 patients in each group. The demographic characteristics of both groups are as described in Table 1. Table 2 shows the difference of mean ONSD and their comparison between propofol and dexmedetomidine infusion in the right and left eye just after creation of pneumoperitoneum (B) and after 15 to 30 minutes of creation of pneumoperitoneum (C). The difference of means of ONSD was greater in dexmedetomidine group and was statistically significant. There was no significant difference in ONSD recorded before pneumoperitoneum ‘A’ and after desufflation of pneumoperitoneum ‘D’ [Table 3].
|
|
Propofol group (n=30) |
Dexmedetomidine group (n=30) |
|
Age (years) (mean±SD) |
46.67±12.06 |
48.26±11.09 |
|
Gender |
|
|
|
Male [n (%)] Female [n (%)] |
10 (33%) 20 (67%) |
7 (23%) 23 (77%) |
|
ASA physical status |
|
|
|
ASA I ASA II |
16 (54%) 14 (46%) |
19 (63%) 11 (37%) |
|
ONSD |
Propofol group |
Dexmedetomidine group |
P value |
|
Right eye (Mean±SD) |
0.02±0.024 |
0.03±0.028 |
0.001 |
|
Left eye (Mean±SD) |
0.025±0.022 |
0.032±0.029 |
0.001 |
|
ONSD |
Propofol group |
Dexmedetomidine group |
P value |
|
Right eye (Mean±SD) |
0.452±0.042 |
0.4560±0.040 |
0.26 |
|
Left eye (Mean±SD) |
0.44±0.037 |
0.45±0.043 |
0.42 |
In this study, the effect of drugs (propofol and dexmedetomidine) on the ONSD of patients undergoing laparoscopic surgeries was examined. The ONSD in both groups increased and exceeded the initial value after the CO2 pneumoperitoneum. The results of the study indicated a significant decrease in ONSD after administration of propofol/dexmedetomidine infusions in both the groups.
Chiara Robba et al, 3 found that the combination of trendelenburg position and pneumoperitoneum position led to elevated intracranial pressure in all non-invasive techniques. Hence, they suggested that individuals undergoing laparoscopic surgery in trendelenburg position should be made aware of the possible risk of developing intracranial hypertension. Our study also concludes that there is a rise in ICP during pneumoperitoneum. Kim et al, 8 analysed the literature and revealed that during laparoscopy there is a significant increase in the ONSD in the early (0-30 min) and late (30-120 min) periods during CO2 pneumoperitoneum. Our findings are supported by this meta-analysis. The effect of propofol and sevoflurane on ONSD was compared by Weilian Geng et al. 9 They found that there was significant change in ONSD, which was more with propofol. The findings of our study are different because sevoflurane is used in both the groups.
Manoj et al. 7 compared the effect propofol, sevoflurane and propofol with dexmedetomidine. It was noted that there was an increase in median ONSD values at 5 min post pneumoperitoneum, and 5 min after trendelenburg position compared to 10 min after intubation. However, there was no significant variation observed in the intergroup comparison among the three groups. The median ONSD values had returned to levels similar to the baseline in all groups. Similar to the above study, we also found increase in ICP intraoperatively and the ICP returns to baseline after desufflation [Table 3]. In 2018 study by Sahay et al. 10 dexmedetomidine showed a slight reduction in the increase of ONSD. Our study also found that dexmedetomidine significantly decreases ONSD. Creation of pneumoperitoneum leads to indirect increase in ICP which is deleterious in the patients who are vulnerable to rise in ICP and its related adverse events. Ultrasonographic ONSD monitoring can be a useful tool to titrate intra-abdominal pressure needed for laparoscopic surgery. 11 Our study also highlights the importance of ONSD monitoring intraoperatively. In a similar study by Sağlam S et al, it has been found that total intravenous anesthesia offers lesser change in ONSD when compared to volatile anesthetic agents.12 We have used both volatile as well as intravenous anesthetic agents, still our findings of significant reduction in ONSD [Table 2] are comparable. İnegöl MÖ et al, compared the effect of sevoflurane and desflurane on intra-cranial pressure. The ICP has been recorded higher in both the groups when compared to baseline. 13 Our findings differ from them because we have included propofol/ dexmedetomidine in our protocol.
Limitations of the study includes: Limited sample size, limited pneumoperitoneum time (60-90 min), single-center study (may yield results that have restricted applicability to a broader population, other factors affecting ICP not taken into account.
We conclude, that in patients undergoing laparoscopic surgery, dexmedetomidine has been found to be a better choice in maintaining ICP as compared to propofol in patients undergoing laparoscopic surgeries of limited duration. However, additional research involving more participants and extended observation periods is necessary to validate these findings.
Subscribe now for latest articles and news.