

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.v11.i3.25.18
Year: 2025, Volume: 11, Issue: 3, Pages: 251-257
Original Article
H Sushma1 , Deepali Valecha2 , Ramyatha Aithal3 , Kishore Kumar Arora4
1Department of Anaesthesiology, Kasturba Medical College, Manipal, Udupi, 576104, Karnataka, India,
2Assistant Professor, Department of Anaesthesiology, MGMMC Indore, Madhya Pradesh, India,
3Assistant Professor, Department of Anaesthesiology, Kasturba Medical College, Manipal, Udupi, 576104, Karnataka, India,
4Professor, Department of Anaesthesiology, Sri Aurobindo Institute of Medical Sciences, Indore, 452010, Madhya Pradesh, India
Address for correspondence: H Sushma, Department of Anaesthesiology, Kasturba Medical College, Manipal, Udupi, 576104, Karnataka, India.
E-mail: [email protected]
Received Date:17 January 2025, Accepted Date:20 March 2025, Published Date:20 October 2025
Background: Attenuation of stress response to direct laryngoscopy and endotracheal intubation is crucial to prevent perianesthetic complications. To lessen this stress response on the body, we compared the effect of oral Pregabalin and Gabapentin, administered preoperatively, on patients undergoing laparoscopic cholecystectomy.
Materials and Methods: This is a prospective, randomized, single-blinded controlled study. Ninenty patients with American Society of Anesthesiologists (ASA) physical status I or II who were scheduled for elective laparoscopic cholecystectomy were enrolled. Random allocation was done in to the three groups, receiving either oral Gabapentin 600 mg, oral Pregabalin 150 mg, or oral placebo, 90 minutes prior to the induction of anesthesia. Monitoring the hemodynamic parameters which included heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP) was done at different time frames.
Results: The groups which received oral Pregabalin and Gabapentin had significantly blunted hemodynamic stress response to direct laryngoscopy and endotracheal intubation compared to the placebo group. There was no statistically significant reduction in heart rate, systolic blood pressure, diastolic blood pressure and mean arterial pressure at baseline or during the preoperative period at 30, 60, or 90 minutes (P > 0.05). Both Pregabalin and Gabapentin groups had statistically significant reduction in heart rate, SBP, DBP, and MAP at 2, 4, 6, 8, and 10 minutes following intubation (p < 0.05).
Conclusion: Both Pregabalin and Gabapentin can effective in attenuating haemodynamic stress response to laryngoscopy and endotracheal intubation in patients undergoing laparoscopic cholecystectomy.
Keywords
Pregabalin, Gabapentin, Stress response, Attenuation
Negotiation of the airway and its instrumentation can cause physiological changes by upsurge in heart rate and blood pressure. As a sequel it may cause deleterious effect on cardiovascular system 1. Physically fit patients will tolerate these sudden fluctuations in haemodynamics but in patients with coronary artery disease, cerebrovascular diseases, this might increase perioperative morbidity and mortality 2.
Laparoscopic procedures cause minimal discomfort, healing is better and lesser chances of complications after surgery than open surgeries. Pneumoperitoneum caused by CO2 insufflation during laparoscopy contributes to significant changes in cardiovascular system, respiratory system and acid-base balance 3. Airway instrumentation with mechanical ventilation is needed for laparoscopic cholecystectomy. The haemodynamic stress response induced by laryngoscopy and endotracheal intubation can be dissipated by deepening the plane of anesthesia and administering different classes of drugs 4.
Relatively newer generation of medication known as gabapentinoids (pregabalin and gabapentin) have analgesic and anxiolytic properties in addition to the primary antiepileptic role. The voltage gated calcium channels have alpha-2-lambda subunits and are extensively dispersed throughout the brain and spinal cord. Pregabalin binds presynaptically to this subunit and alters calcium current to decrease or modify the release of multiple excitatory neurotransmitters (norepinephrine, substance P, glutamate and calcitonin gene related peptides) 5, 6. This reduces the hyperexcitability of dorsal horn neurons caused by tissue injury.
Gamma Amino Butyric Acid is similar to gabapentin. It is neither an agonist nor an antagonist, despite being a GABA analog. It acts by binding to the α2d subunit of voltage gated calcium channels, which decreases the release of few excitatory neurotransmitters. Without changing the substance, gabapentin also suppresses the release of catecholamines from the adrenal medulla 7.
A literature search revealed paucity of data that compared the aforementioned study drugs and their efficacy in attenuating pressor response. Thus, this study compares the effects of gabapentin and pregabalin in the reducing stress response during endotracheal intubation and laryngoscopy in patients undergoing Laparoscopic cholecystectomy.
This is a prospective, randomized, single-blinded study which was conducted in the Department of Anesthesiology at Tertiary care centre in Central India. The study was conducted after obtaining approval from the Institutional ethics and scientific Committee (EC/MGM/Feb-20/33). Randomisation was done by chit box method into three groups. Group P received Oral pregabalin 150mg, group G received oral gabapentin 600mg, Group C received placebo (Vitamin B complex). A total of 90 patients who were posted for laparoscopic cholecystectomy under general anaesthesia were recruited.
Patients included in the study were ASA physical status I or II, either sex belonging to age group of 18-65 year and those with intubation duration less than 15 seconds, and patients undergoing laparoscopic cholecystectomy under general anesthesia. Patients with anticipated difficult intubations, multiple intubation attempts (more than one), with duration of laryngoscopy exceeding 20 seconds, ASA physical status III or IV, known allergy to Pregabalin or Gabapentin, and patients on tricyclic antidepressants, chronic neuroleptic medications, SSRIs, and lastly, patients who refused to consent for this study were excluded.
On a day prior to the surgery, all the patients underwent a pre-anesthetic assessment and were briefed about the study protocol. They were instructed to remain nil by mouth from midnight. On the day of surgery, patients were randomly allocated into their respective groups and given their oral medications 90 minutes prior to the surgery. Patients were monitored in preoperative room every 30 minutes.
After shifting them to the operating room, baseline line parameters such as systolic (SBP), diastolic (DBP) and mean blood pressures (MBP) were noted along with pulse rate, oxygen saturation (SpO2) and electrocardiogram. Ringer lactate solution was started through 18G cannula via peripheral vein. General anesthesia was induced with Inj. Fentanyl iv 2 mic/kg, Inj Propofol in titrated dose and Inj Atracurium iv 0.5mg/kg loading dose was given. Airway was secured with appropriately sized cuff endotracheal tube. Outcome parameters (HR, SBP, DBP, MBP) were recorded during intubation and laryngoscopy as well as 2, 4, 6, 8, 10min post intubation. Other vital monitors including end tidal carbon dioxide monitoring was continued throughout the surgery. After the completion of the surgical procedure, patient was extubated after adequate neuromuscular blockade reversal.
We used the formula N= [a2 ×S2×2] / d2 to estimate the sample size where, ‘a’ is the coefficient of difference (1.96), S, obtained from the previous study (0.34), and ‘d’ is the degree of differentiation (10%). After formulating a sample size of 90 was obtained. GraphPad InStat v3.0. was used for the data analysis. Frequency and percentages were used to depict all categorical data, while mean and standard deviation or median and interquartile range, depending on the distribution, was used to describe any continuous data.
After verifying the normalcy assumption, the Independent Mann-Whitney U test or Sample t-test was used for continuous variables to compare the continuous data. Fisher's exact test or Chi-square test was used for categorical variables based on the expected frequency. For every comparison, the p value was considered significant at 5% (0.05).
The demographic variables in all three groups were comparable and statistically insignificant (p >0.05). The details are illustrated in Table 1.
|
Clinico-demographic variable |
Parameter |
Group P (n=30) |
Group G (n=30) |
Group C (n=30) |
P-value |
|
Age in years |
Average age (Mean ± SD) |
39.73 ± 13.55 |
38.67 ± 13.33 |
41.03 ± 5.62 |
0.72 |
|
Gender distribution |
Male |
6 (20%) |
7 (23.3%) |
8 (26.7%) |
0.83 |
|
Female |
24 (80%) |
23 (76.7%) |
22 (73.3%) |
||
|
Duration of surgery in minutes |
Average time (Mean ± SD) |
135.17 ± 11.33 |
132.50 ± 8.17 |
130.40 ± 6.14 |
0.116 |
|
ASA grade |
ASA I |
24 (80%) |
27 (90%) |
22 (73.3%) |
0.25 |
|
ASA II |
6 (20%) |
3 (10%) |
8 (26.7%) |
||
|
Side-effect profile |
None |
26 (86.7%) |
28 (93.3%) |
30 (100%) |
0.36 |
|
Dizziness |
2 (6.7%) |
1 (3.3%) |
0 |
||
|
Nausea |
2 (6.7%) |
1 (3.3%) |
0 |
Baseline Heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP) were measured. Thereafter they were measured at 30 minutes, 60 minutes, and 90 minutes before surgery, and then at 2, 4, 6, 8, and 10th minute post induction.
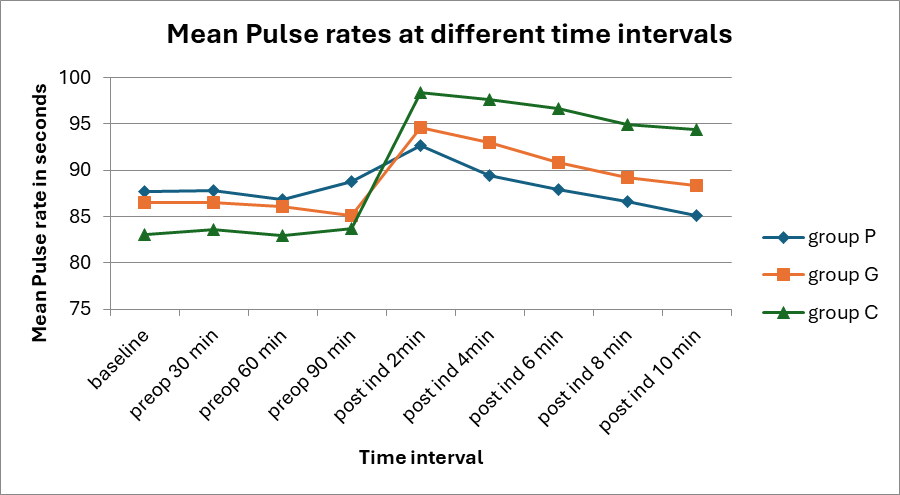
Baseline vitals were comparable in all the three groups. Group C showed significantly higher heart rate at 2, 4, 6, 8, and 10 minutes after induction compared to Groups G and P. The heart rate at 2, 4, 6, 8 and 10 minutes after induction in Groups P and G were similar, with no statistically significant difference between them (p> 0.05). Table 2 and Figure 2 represent the heart rate at different time intervals among the three groups.
|
Time point |
Group P Mean ± SD |
Group G Mean ± SD |
Group C Mean ± SD |
P value |
|
Baseline |
87.70 ± 8.59 |
86.50 ± 7.70 |
83.07±9.93 |
0.112 |
|
Preop 30 min |
87.80 ± 7.46 |
86.53 ± 7.40 |
83.57±10.27 |
1.969 |
|
Preop 60min |
86.87 ± 8.08 |
86.13 ± 6.86 |
83.00±9.44 |
1.885 |
|
Preop 90min |
88.77 ± 7.65 |
85.13 ± 7.30 |
83.73±10.77 |
2.666 |
|
Post induction 2 min |
92.67 ± 6.45 |
94.63 ± 3.74 |
98.43±4.76 |
0.001* |
|
4 min |
89.47 ± 7.24 |
92.97 ± 3.71 |
97.67±3.33 |
0.001* |
|
6 min |
87.87 ± 8.04 |
90.87 ± 4.14 |
96.70±3.96 |
0.001* |
|
8 min |
86.57 ± 7.23 |
89.20 ± 4.35 |
94.90±4.11 |
0.001* |
|
10 min |
85.07 ± 6.78 |
88.37 ± 4.43 |
94.37±4.51 |
0.001* |
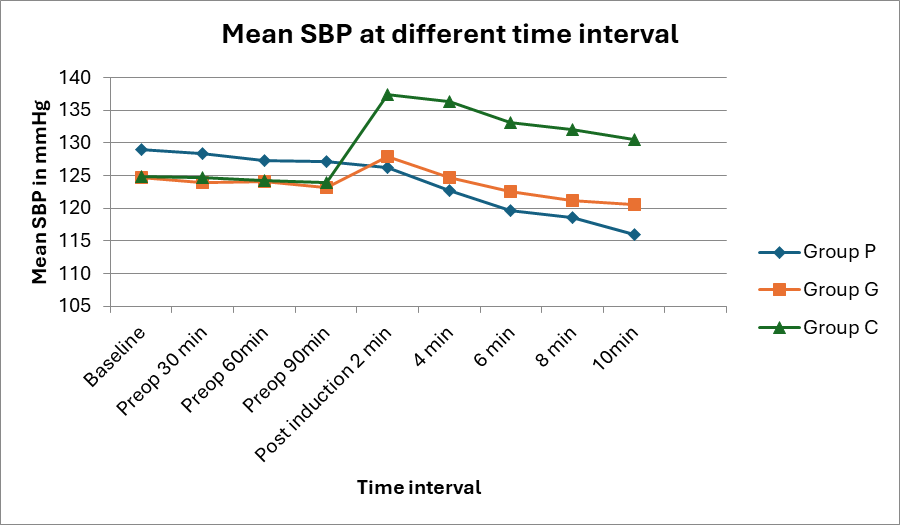
Group C exhibited a statistically significant increase in SBP and DBP at 2, 4, 6, 8, 10 minutes post-induction compared to Groups P and G (p < 0.05). However, during the preoperative time frames, SBP was comparable across all three groups. This data is represented in Figure 3, Figure 4 and Table 3.
|
Haemodynamic variable |
Time point |
Group P Mean ± SD |
Group G Mean ± SD |
Group C Mean ± SD |
P value |
|
Systolic blood pressure |
Baseline |
128.93 ± 11.09 |
124.73 ± 5.99 |
124.90±9.73 |
0.140 |
|
Preop 30 min |
128.30 ± 10.78 |
123.97 ± 5.90 |
124.63±8.64 |
0.120 |
|
|
Preop 60min |
127.33 ± 11.19 |
124.07 ± 5.04 |
124.17±8.64 |
0.257 |
|
|
Preop 90min |
127.17 ± 10.39 |
123.10 ± 4.91 |
123.90±8.29 |
0.131 |
|
|
Post induction 2 min |
126.23 ± 8.14 |
127.97 ± 6.44 |
137.43±6.98 |
0.001* |
|
|
4 min |
122.70 ± 7.59 |
124.70 ± 5.91 |
136.40±6.88 |
0.001* |
|
|
6 min |
119.63 ± 8.21 |
122.53 ± 6.09 |
133.13±6.92 |
0.001* |
|
|
8 min |
118.53 ± 8.68 |
121.23 ± 6.97 |
132.03±6.01 |
0.001* |
|
|
10 min |
115.93 ± 8.66 |
120.57 ± 6.25 |
130.47±6.00 |
0.001* |
|
|
Diastolic blood pressure |
Baseline |
82.80 ± 6.58 |
80.03 ± 6.39 |
80.20±6.47 |
0.185 |
|
Preop 30 min |
82.17 ± 5.75 |
79.50 ± 6.83 |
78.77±6.65 |
0.464 |
|
|
Preop 60min |
81.00 ± 7.97 |
80.17 ± 6.35 |
78.50±5.78 |
0.063 |
|
|
Preop 90min |
81.70 ± 6.25 |
80.30 ± 5.65 |
78.77±5.29 |
0.148 |
|
|
Post induction 2 min |
81.00 ± 7.31 |
83.50 ± 6.89 |
88.83±5.45 |
0.001 |
|
|
4 min |
78.43 ± 6.15 |
81.20 ± 5.70 |
88.57±5.50 |
0.001 |
|
|
6 min |
76.77 ± 7.04 |
77.93 ± 5.31 |
85.40±6.32 |
0.001 |
|
|
8 min |
75.93 ± 7.83 |
78.83 ± 5.69 |
83.57±6.34 |
0.001 |
|
|
10 min |
73.17 ± 5.98 |
77.40 ± 6.04 |
82.47±6.01 |
0.001 |
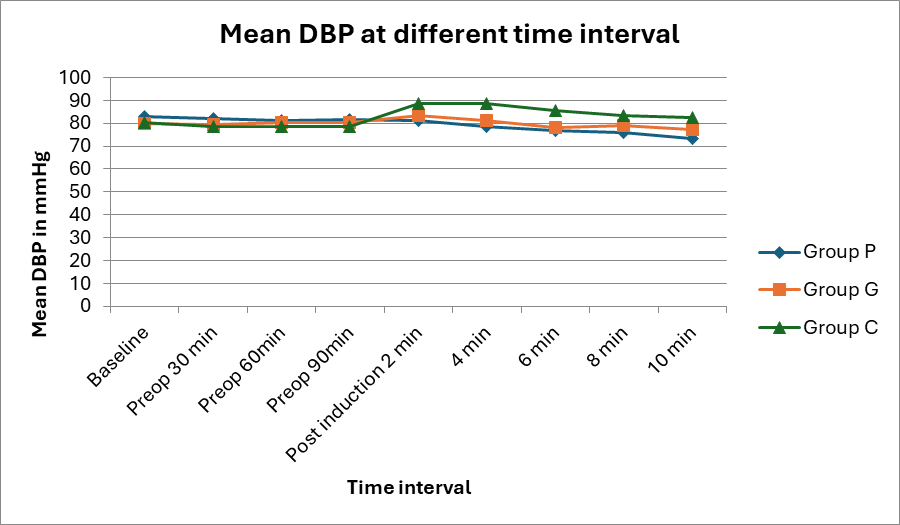
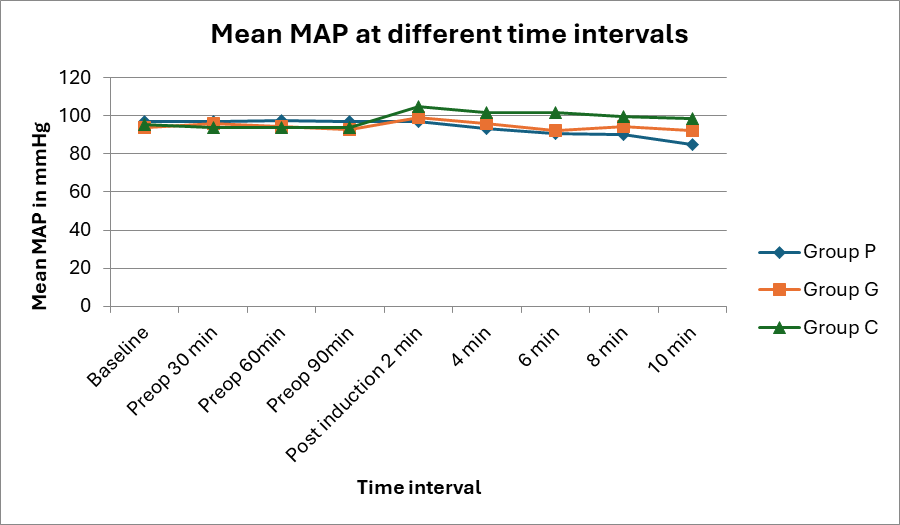
A similar trend in MAP was noted, where a significant increase in mean arterial pressure was observed in group C at 2, 4, 6,8 ,10 minutes post-induction compared to Group P and G (p < 0.05). The mean MAP for each group is shown in Table 4 and Figure 5.
|
Time point |
Group P Mean ± SD |
Group G Mean ± SD |
Group C Mean ± SD |
P value |
|
Baseline |
97.07 ± 8.50 |
94.00 ± 6.39 |
95.20±6.93 |
0.269 |
|
Preop 30 min |
96.87 ± 8.34 |
95.63 ± 7.05 |
93.83±6.09 |
0.268 |
|
Preop 60min |
97.33 ± 7.39 |
94.33± 6.26 |
93.67±5.83 |
0.074 |
|
Preop 90min |
96.80 ± 7.22 |
92.50 ± 16.56 |
93.77±5.34 |
0.295 |
|
Post induction 2 min |
96.70 ± 7.47 |
98.83 ± 7.59 |
104.90±5.18 |
0.001* |
|
4 min |
93.10 ± 6.14 |
95.67 ± 7.68 |
101.47±17.24 |
0.001* |
|
6 min |
90.83 ± 6.66 |
92.17 ± 6.54 |
101.53±5.89 |
0.001* |
|
8 min |
90.30 ± 8.57 |
94.23 ± 6.12 |
99.73±5.71 |
0.001* |
|
10 min |
84.97 ± 14.08 |
92.07 ± 5.23 |
98.43±5.46 |
0.001* |
Patients with cardiovascular and cerebrovascular disorders may suffer from the cardiovascular reflexes caused by the unpleasant stimulus of laryngoscopy and intubation, such as tachycardia and hypertension 8. Nonopioid medications are being used as a part of the multimodal regimen to ease anxiety and the intubation response. Our study assessed the effect of Pregabalin and Gabapentin in reducing the stress response to laryngoscopy and endotracheal intubation in patients undergoing laparoscopic cholecystectomy under general anaesthesia. Pregabalin is an anticonvulsant, analgesic, and antianxiety medication that is primarily used to treat neuropathic pain, post herpetic neuralgia, and partial onset seizures as an adjuvant. The original purpose of gabapentin and pregabalin was to treat epilepsy and effectively control neuropathic pain. Additionally, they are employed to relieve discomfort during the perioperative period 9.
In our study, the demographic profiles of all the three groups were comparable. There was no significant difference in heart rate among the three groups before induction. However, after induction, Group C showed a significant increase in heart rate compared to Group G and Group P, with this difference being statistically significant at 2, 4, 6, 8, and 10 minutes (P = 0.001). Groups P and G were comparable in this regard. This finding supports a study by Namratha Urs et al 10, who evaluated the efficacy of oral Pregabalin and Gabapentin in attenuating the haemodynamic stress response to laryngoscopy and intubation in patients undergoing general anesthesia. In their study, the baseline and pre induction heart rate values were comparable, while there was a significant reduction in heart rate at 0, 1 and 3 minutes post induction.
The diastolic blood pressure (DBP) values in our study were comparable among all the groups at baseline. The mean DBP across the three groups before induction at 30, 60, and 90 minutes was also similar and not statistically significant (P > 0.05). However, following induction, Group C showed a significant increase in DBP compared to Group P and Group G at 2, 4, 6, 8, and 10 minutes, with the difference being statistically significant (P = 0.001). These findings are similar to the results of a study by Doddaiah et al 11, where the effect of oral Pregabalin (150 mg) and Gabapentin (800 mg) given preoperatively were evaluated. Their study demonstrated a statistically significant reduction in DBP in the Gabapentin group at 1 and 5 minutes compared to the control group which received placebo. Similarly, a significant reduction in DBP was observed in the Pregabalin group compared to the control group at 1, 5, 10, and 15 minutes. DBP values between the Pregabalin and Gabapentin groups were found to be comparable.
Groups P, C, and G had similar baseline mean arterial pressures. The readings following drug use were statistically not significant and comparable to the baseline levels. During laryngoscopy and 2, 4, 6, 8,10 minutes after intubation, Group C had the highest mean MAP compared to Groups P and G. This difference was found to be statistically significant (P=0.01). Group P and Group G had similar mean MAPs. These findings are similar to a study by Ramya et al 12, where there was a statistically significant decrease in MAP upon induction at 0, 1, 3, 5, and 10 minutes compared baseline in the Pregabalin and Gabapentin groups. In both pregabalin and gabapentin groups, the mean MAP were similar. Namratha S Urs et al10 also found that at 0, 1, 3, and 5 minutes after intubation, the MAP in the Gabapentin and Pregabalin groups was statistically significantly lower than that of the Control Group. The groups using pregabalin and gabapentin showed similar MAP changes. Eren et al13 evaluated pregabalin in attenuating the hemodynamic response to intubation in lumbar surgeries among 50 patients undergoing elective lumbar disc surgery. They noticed that the mean MAP values were significantly lower in pregabalin 150 group than those of the placebo group (108.3 ± 6.3 vs. 119.4 ± 9.8, P = 0.0001) during laryngoscopy and intubation, lasting ten minutes. The pregabalin 150 mg group's mean MAP increased from baseline by 9%, while the placebo group's mean MAP increased by 23%.
Our study had several limitations, mainly in its single center design and small sample size. Although the duration of laryngoscopy was restricted to less than 15 seconds, the duration of laryngoscopy was not noted. The study was limited to patients with ASA Grade I and II, excluding patients with comorbidities, who may not tolerate pressor responses. Future research is recommended in a multicenter setting with a larger sample size and the inclusion of patients with comorbidities to provide more comprehensive findings.
From the current study, we concluded that, Pregabalin 150 mg and Gabapentin 600mg given orally prior to surgery is effective in attenuating the stress response for Laryngoscopy and endotracheal Intubation.
Funding: None
Conflict of Interest: None
Subscribe now for latest articles and news.